Prompt Diagnosis by MHS Improves Survival

A patient at Naval Hospital Pensacola prepares to have a low-dose computed tomography test done to screen for lung cancer. Lung cancer is the leading cause of cancer-related deaths among men and women. Early detection can lower the risk of dying from this disease. Navy photo by Jason Bortz
BETHESDA, MD — Lung cancer remains the leading cause of cancer death in the United States, killing more than 150,000 people each year. Lung cancer also poses a particularly high risk to servicemembers and veterans.
Some of the risk of developing lung cancer comes with the job. Military personnel are more frequently exposed to environmental carcinogens than most other Americans. Some of the risk comes from behaviors more common in current and former servicemembers, such as smoking, which causes about 85% of all lung cancers.
The high death rate from lung cancer, however, arises from the malignancy’s stealthy nature and there, recent research indicates, serving in the military appears to provide an advantage.
Lung cancer often progresses with few signs or symptoms until patients have reached an advanced stage of the disease. That has a huge impact on patient mortality. Among individuals with non-small cell lung cancer (NSCLC), the most common type of lung cancer, those with localized disease have a five-year relative survival rate of 55.6%. In comparison, only 4.5% of patients with distant metastases at diagnosis live for another five years.
Long-term survival depends on early diagnosis—and military service appears to provide an edge in that regard. While individuals in the military are more likely to develop lung cancer than the general population, they are also more likely to be diagnosed at an early point in their disease and to have better overall outcomes, according to a recent study published in Military Medicine by researchers at the John P. Murtha Cancer Center Research Program at the Uniformed Services University of the Health Sciences (USUHS) in Bethesda, MD.1
The team, led by Joel Anthony Nations, MD, chief of medicine at the Walter Reed National Military Medical Center and the USUHS, compared 21,031 patient records in the DoD Automated Central Tumor Registry (ACTUR) to data on 773,356 patients in the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute. All patients received a diagnosis of NSCLC between 1989 and 2012.
 The racial composition of the two populations were similar. ACTUR had a higher proportion of men (65.3%) than SEER (55.1%). Military patients developed lung cancer at a younger age than the general population with 7.3%, 60.0%, and 32.7% of individuals in ACTUR less than age 50, age 50 to 69, or age 70 or older, respectively, compared to 5.6%, 45.8% and 48.9% for the same age groupings in SEER.
The racial composition of the two populations were similar. ACTUR had a higher proportion of men (65.3%) than SEER (55.1%). Military patients developed lung cancer at a younger age than the general population with 7.3%, 60.0%, and 32.7% of individuals in ACTUR less than age 50, age 50 to 69, or age 70 or older, respectively, compared to 5.6%, 45.8% and 48.9% for the same age groupings in SEER.
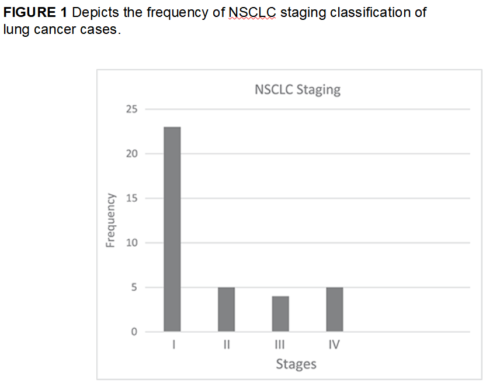
In both populations, the largest group of patients had Stage 4 disease at diagnosis, but a notably lower percentage of military patients had metastases, 33.6%, compared to 40.5% for those in the SEER database. Patients presented with Stages 3 and 2 disease at very similar rates in both the ACTUR and SEER databases, 26.1% vs. 26.44%, respectively, for Stage 3, and 5.6% and 4.0%, respectively, for Stage 2. Nearly one-quarter of military patients (24.7%) received their NSCLC diagnosis while still in Stage 1, compared to 1 in 5 patients (20.6%) in the general population.
Overall, 10% of ACTUR patients and 8.44% of SEER cases had an unknown stage at diagnosis. The percentage of unknown stage patients in ACTUR steadily declined throughout the duration of the study, dropping from 14% in 1989 to 2003 to 5.1% for the 2009 to 2012 period. Unknown cases in SEER varied from year to year.
In interpreting their findings, the researchers proposed that the “universal care model of the MHS might allow beneficiaries to seek medical care earlier and lead to earlier stages of cancer diagnoses.” Other studies have demonstrated that access to medical care strongly influences lung cancer stage at diagnosis.
Previous research by the team also demonstrated that lung cancer patients care for within the MHS had better survival rates than the general population. They attributed reduced mortality in part to higher rates of surgery for patients with Stage 1 and 2 disease and greater use of radiation therapy for Stage 3 and 4 patients and to the cancer care team model used by the MHS.2 The current study’s findings suggest that higher rates of early diagnosis also play a role in improved survival.
Improved Survival
Two developments have likely further improved both the rate of early diagnosis and survival in servicemembers in recent years. The time period covered by the study, 1989 to 2012, predates the first guidelines issued by the U.S. Preventive Services Task Force (USPSTF) for screening for lung cancer in high-risk patients. The past five years have also seen an explosion in the options for treating lung cancer.
Since 2013, USPSTF has recommended low-dose computed tomography lung cancer screening or patients aged 55 to 80 who have a 30-pack-year history (number of packs per day times number of years smoked) and are current smokers or quit smoking within the previous 15 years. The National Lung Screening Trial, which prompted the guidelines, demonstrated that screening high-risk patients reduced mortality 20%. A subsequent large study, the NELSON trial, showed even greater benefit, a 26% reduction in mortality in men and a 66% mortality reduction in women.
The screening recommendations have been adopted across the DoD with significant success, perhaps facilitated by mandated annual physicals. The Naval Medical Center San Diego (NMCSD), for instance, implemented its screening program in September 2013 and screened 962 patients within five years.
Fourteen percent of patients screened had a positive screening test, Lung-RADS score of 3 or 4, that prompted further investigation. The screening detected lung cancer in 43 individuals, with 37 of them having NSCLC and five categorized as small cell lung cancer. Another 21 patients were pending repeat imaging at the time of a recent study. Of the confirmed NSCLC patients, 76% were diagnosed at Stage 1 or 2, 11% at Stage 3, and just 13% at Stage 4.3
The numbers from the NMCSD study indicate that the percentage of servicemembers diagnosed with early stage NSCLC has more than doubled since the implementation of screening.
That may be just the beginning of the good news.
“In my clinic, I have more survivors today than I had years ago,” said Karen Zeman, MD, an oncologist at Walter Reed National Military Medical Center in Bethesda, MD. “The lung cancer patients are doing significantly better in 2020 than they were doing in 2014.”
That’s because the U.S. Food and Drug Administration has approved dozens of new lung cancer drugs in in recent years. The DoD is part of the APOLLO federal initiative with the National Institutes of Health and the Department of Veterans Affairs working to further the understanding of the genetic mutations involved in cancer that has underpinned many of the new drug discoveries. That understanding could also allow screening to be even more targeted.
“The APOLLO project is mainly focused on active duty military servicemembers in the DoD and veterans,” said Robert Browning, MD, medical director of interventional pulmonary at WRNMMC. “We’re going to find some answers about lung cancer in the military and the DoD, among other cancers, that just were not possible before this project.”
For physicians and patients in the MHS, these developments offer better outcomes than many could have imagined a decade ago, and more are on the horizon.
“Lung cancer is a terrible diagnosis, but if there’s any message to get to lung cancer patients diagnosed now, it’s to hang on because there are treatments coming at a pace we have never seen in our lives or in history,” Browning said. “We all were trained in treating lung cancer that had the same death rate for the past 50 years. And then, in the past five years, things have exploded and we’ve made tremendous progress.”
- Nations JA, Brown DW, Shao S, Shriver CD, Zhu K. Comparative Trends in the Distribution of Lung Cancer Stage at Diagnosis in the Department of Defense Cancer Registry and the Surveillance, Epidemiology, and End Results data, 1989-2012. Mil Med. 2020 Aug 28:usaa218. doi: 10.1093/milmed/usaa218. Epub ahead of print. PMID: 32857164.
- Lin J, Kamamia C, Brown D et al: Survival among lung cancer patients in the U.S. military health system: a comparison with the SEER population. Cancer Epidemiol Biomarkers Prev. 2018;27(6): 673–9.
- White LJ, Kaur A, Lapel RT, Boswell GE, Luceri RE, Parrish JS, Seda G. Lung Cancer Screening at a Military Treatment Facility: A Retrospective Review. Mil Med. 2020 Jun 8;185(5-6):e864-e869. doi: 10.1093/milmed/usz386.
