Veterans Study Finds Issues Goes Beyond Opioids
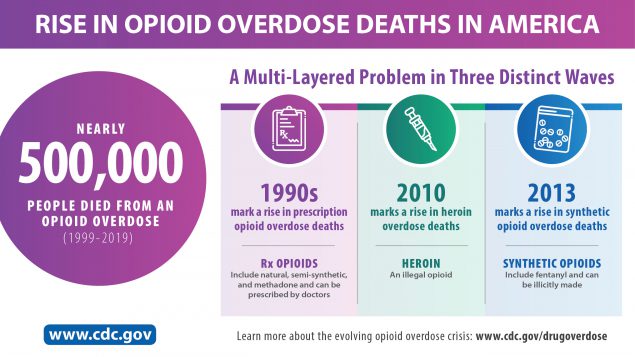
ANN ARBOR, MI — Fatal drug overdoses have surpassed automobile accidents in recent years as the leading cause of accidental death and, despite efforts to reverse that trend, the number of overdoses is rising.
While opioids have been a key focus of overdose and treatment efforts—with the U.S. Department of Health and Human Services declaring the opioid epidemic a public health emergency in 2017—a new VA study confirms that opioids are only part of this growing problem. The study shows a dramatic increase in stimulant-involved overdoses in recent years, with the majority of these overdose deaths involving multiple substances.
“There’s been so much focus on the opioid overdose epidemic that the role of other substances has been overshadowed,” said Lara Coughlin, PhD, assistant professor at the University of Michigan Addiction Center in the Department of Psychiatry and lead author of the study which was published in Addiction. “In this study, we look at overdose deaths that involved stimulants, including overdoses involving cocaine and methamphetamine. We were also interested in characteristics of people who died from different types of stimulant overdoses to help inform where to target substance use treatment and overdose prevention efforts.”1
In the study, which also involved the VA’s Center for Clinical Management Research (CCMR) in Ann Arbor, researchers linked National Death Index data, including date and cause of death, from the National Vital Statistics System mortality files with VHA patient data. Individuals were included in the cohort if they had at least one in- or out-patient VHA encounter in the year prior to an overdose death, were aged 18 years or older and died from a stimulant-involved overdose during calendar years 2012-18.
Types of overdose deaths were classified using the International Classification of Diseases, 10th revision (ICD-10) and, based on toxicology results, were categorized in one of six ways: (1) cocaine only, (2) methamphetamine only, (3) cocaine + opioid, (4) methamphetamine + opioid, (5) stimulant + other nonopioid substance and (6) both cocaine + methamphetamine, with or without opioids. Demographic and patient characteristics, obtained from VHA records, include age, sex, race, ethnicity, homelessness status, geographic locality (urban/rural), primary location and utilization of care, comorbid diagnoses and reported prescription refills from VHA pharmacies for central nervous system-active drugs in the year prior to an overdose death.
Fatal overdoses per year for each of the six stimulant-involved overdose profiles were computed and plotted to show trends from 2012 to 2018.
Stimulants Involved
More than one-fourth of the overdose deaths involved stimulants, the study found, with the rate of stimulant-involved overdoses tripling from 2012 to 2018. In total, 3,631 veterans died from stimulant-involved overdoses, compared to 9,353 veterans who died from opioid-involved overdoses during the same period.
Other key findings:
- Of stimulant-involved overdose deaths, 857 veterans in the National Death Index database died of cocaine alone and 755 of methamphetamine alone; however, 54.1% (1965) of all stimulant-related overdoses also involved an additional substance.
- Of opioid-involved overdoses, 45.0% involved heroin, 46.1% involved synthetic opioids (e.g., fentanyl) and 25.9% involved prescription opioids. Type of opioid significantly differed by stimulant type. “Of people who died from co-involved stimulant and opioid overdoses, overdoses involving cocaine more often included synthetic opioids whereas overdoses involving methamphetamine more often included prescription opioids,” Coughlin noted.
- “Other substances” were documented in 31.2% of stimulant + opioid overdoses. Alcohol was the most common additional substance, documented in 18.4% of stimulant + opioid deaths.
Several social demographic factors distinguished between overdose types, the study found. For example, fatal overdoses from methamphetamine compared to cocaine were more frequent among younger veterans. Overdoses that involved both stimulants and opioids were also more common in younger veterans compared to overdoses involving only stimulants, regardless of stimulant type.
People who identified as non-Hispanic, Black were overrepresented relative to VHA racial and ethnic composition, specifically among those who died of cocaine-involved fatal overdose. “This may reflect the intersection of differences in cocaine use by race with racial disparities in social determinants of health,” the authors wrote.
Veterans in rural areas had a greater risk of fatal overdose from methamphetamine compared to cocaine with or without co-involved opioids. “This finding fits within the context of methamphetamine being more prevalent, easily accessible, available at a low cost, and perceived as less harmful and stigmatized compared to other illicit drugs such as heroin in rural areas,” the authors wrote.
“These patterns indicate there may be distinct subgroups and patterns of substance use,” said Coughlin. “Highlighting the need to target and tailor our treatment and prevention efforts to particularly high-risk populations taking into consideration differences in contexts, characteristics, substance use patterns, etc.”
- Coughlin LN, Zhang L, Bohnert ASB, Maust DT, Goldstick J, Lin L. Patient characteristics and treatment utilization in fatal stimulant-involved overdoses in the United States Veterans Health Administration. Addiction. Oct. 14, 2021. doi.org/10.1111/add.15714