Study Suggests Difference is Explained by ‘Unique Local Factors’
PITTSBURGH, PA — Low-value diagnostic testing not only is associated with wasteful healthcare spending but also has the potential to expose patients to risk with little benefit.
New researcher involving more than a million veterans raised questions about the frequency and degree of variation in low-value diagnostic testing at the VHA, specifically focusing on low back pain, headache, syncope, and sinusitis.
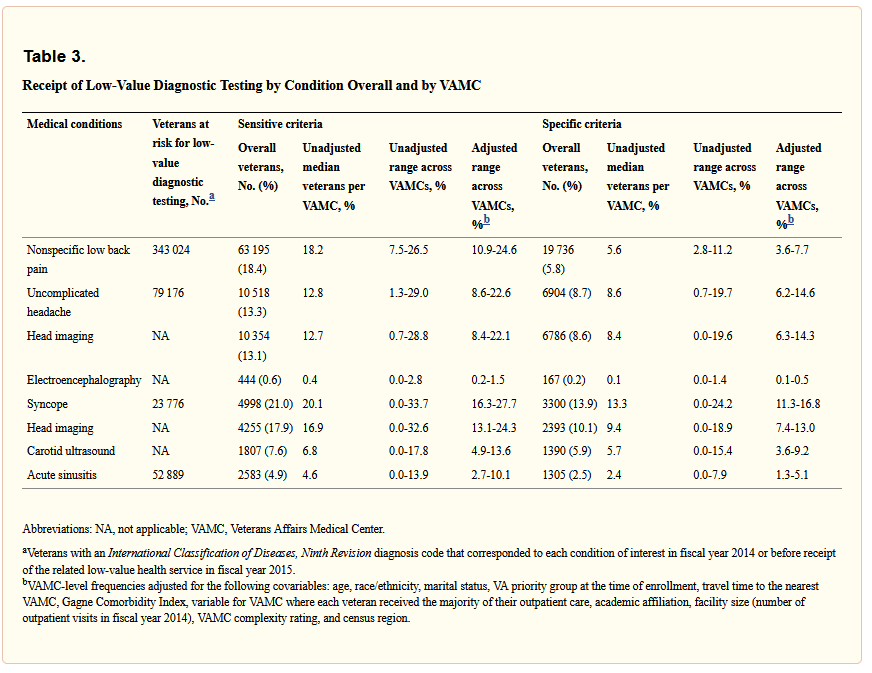
The report in JAMA Network Open found that low-value testing was performed for 5% to 21% of veterans with 1 of the 4 medical conditions, although the use of low-value testing varied substantially across VAMCs.1
Researchers from the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System and the University of Pittsburgh School of Medicine said their findings suggested “the need to address the delivery of such care, even in integrated health systems, with robust decision support and utilization management.”
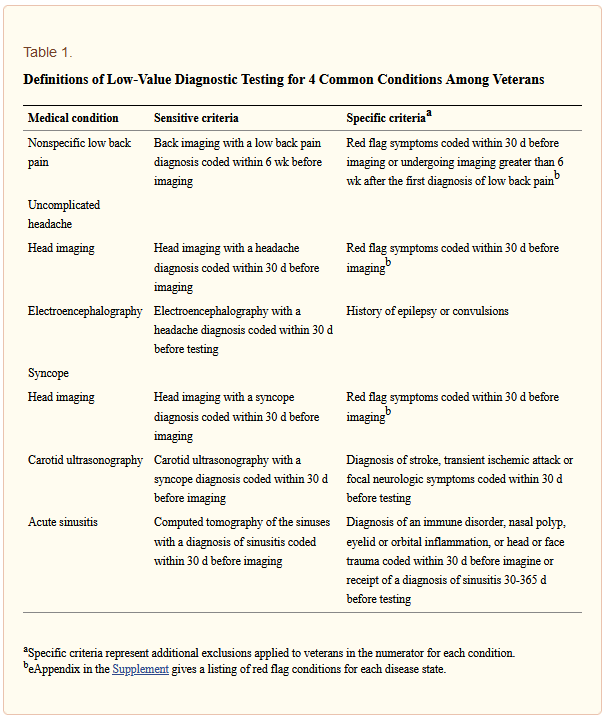
This retrospective cohort study used VHA data from 127 VAMCs from fiscal years 2014 to 2015, with analysis from April 2018 to March 2020.For each condition, sensitive and specific criteria were used to evaluate the overall frequency and range of low-value testing, adjusting for sociodemographic and VAMC characteristics.
The 1,022,987 patients had a mean age of 60, with most, 92.4% male. More than two-thirds, 69.8%, were non-Hispanic white. During the study period, 343,024 veterans (31.4%) were diagnosed with low back pain, 79,176 (7.3%) with headache, 23,776 (2.2%) with syncope, and 52,889 (4.8%) with sinusitis.
“With the sensitive criteria, overall and VAMC-level low-value testing frequency varied substantially across conditions: 4.6% (range, 2.7%-10.1%) for sinusitis, 12.8% (range, 8.6%-22.6%) for headache, 18.2% (range, 10.9%-24.6%) for low back pain, and 20.1% (range, 16.3%-27.7%) for syncope,” the authors reported.
The study points out that, with the specific criteria, the overall frequency of low-value testing across VAMCs was:
-
2.4% (range, 1.3%-5.1%) for sinusitis,
-
8.6% (range, 6.2%-14.6%) for headache,
-
5.6% (range, 3.6%-7.7%) for low back pain, and
-
13.3% (range, 11.3%-16.8%) for syncope.
The study noted that median adjusted odds ratio ranged from 1.21 for low back pain to 1.40 for sinusitis. At VAMCs, low-value testing was most strongly correlated for syncope and headache (ρ = 0.56; P < .001) and low back pain and headache (ρ = 0.48; P < .001), researchers wrote.
Background information in the article described wasteful healthcare spending makes up as much as United States, about 25% of the nation’s total health care expenditures. The authors advised that more than $100 billion has been spent on low-value care, which is defined as the use of health services for which immediate or downstream harms or costs exceed the potential benefits.
Common examples of low-value care include cancer screening for patients with a limited life span or performing preoperative electrocardiography for patients undergoing low-risk cataract surgery. Past research has demonstrated that as many as 43% of Medicare beneficiaries have received low-value care. The downsides, according to the authors, include physical and psychological harm and an erosion of trust in the healthcare system.
“Although the delivery of multiple specific low-value health services has been described among Medicare and private insurance beneficiaries, the use of such services in the Veterans Health Administration (VHA) has not been well characterized,” according to the report.
Practice Environment
While VHA is the largest integrated and federally operated health care system in the United States it has a very different practice environment than other systems, and the researchers sought to determine how that affected the provision of low-value care.
“For example, VHA clinicians do not operate within a fee-for-service system and are insulated from malpractice litigation,” they wrote. “Moreover, the VHA electronic medical record contains information on veterans’ care across all Veterans Affairs Medical Centers (VAMCs) and decision support tools for ordering appropriate health services, which may be associated with a decreased likelihood of VA clinicians delivering low-value care.”
Despite that, the authors pointed out, studies f on the use of individual low-value health services – specifically prostate cancer screening and colonoscopy –have documented the provision of low-value care at VAMCs.
“As health care costs continue to increase and recent legislation provides veterans with increasing flexibility regarding whether they receive care within or outside the VHA, quantifying the frequency and patterns of low-value care delivery is essential for the VHA to reduce wasteful health care spending without compromising quality or patient satisfaction,” they emphasized.
Researchers said their results are in line with prior studies examining multiple low-value diagnostic tests. The goal was to expand understanding of the scope and variability of low-value testing throughout the VHA.
“Our findings are notable in that VA clinicians are not subject to the same incentives and circumstances commonly associated with low-value testing in non-VA settings in the US,” the article stated. “For example, unlike VA physicians who are federal employees, non-VA clinicians may be financially incentivized for ordering certain health services, especially if they own the related equipment. VA physicians are also insulated from malpractice lawsuits and have access to an electronic medical record system that contains records from the entirety of the VHA system and incorporates decision-support tools, enhancing the ability of physicians to make clinical decisions. Furthermore, the variation that we observed in low-value testing across VAMCs could not be easily explained by the traditional veteran- and VAMC-level covariates that we incorporated in our analyses.”
That lead to the conclusions that “unique local factors, such as those related to provider culture and variations in the robustness of decision support for ordering tests and procedures at each VAMC” led to variations in low-value testing.
“The correlations of the receipt of low-value testing among the health conditions in our study also suggest that the delivery of such care at VAMCs is associated with systemic factors that are not specific to the delivery of an individual test,” the authors wrote.
The question, they added, is how to turn the situation around, explaining, “To the extent that low-value care delivery is specific to certain tests and procedures, directed interventions and decision-support tools integrated within the electronic medical record system may be sufficient to reduce the delivery of such care. Although the development of additional service-specific interventions is appropriate in certain circumstances, addressing those latent factors associated with the overarching provision of low-value care may require the institution of broad cultural change targeted at the national and VAMC levels. To aid in this task, our claims-based approach to identify low-value testing may help the development of future value-based metrics.”
- Radomski TR, Feldman R, Huang Y, Sileanu FE, Thorpe CT, et. Al. Evaluation of Low-Value Diagnostic Testing for 4 Common Conditions in the Veterans Health Administration. JAMA Netw Open. 2020 Sep 1;3(9):e2016445. doi: 10.1001/jamanetworkopen.2020.16445. PMID: 32960278; PMCID: PMC7509631.