By Mary Anne Dunkin
CHICAGO — In the last decade, the U.S. Centers for Medicare and Medicaid Services (CMS) and the Veterans Health Administration (VHA) have prioritized reducing avoidable hospital readmissions. Yet, policies intended to incentivize hospitals to reduce readmissions in people with chronic obstructive pulmonary disease (COPD) have produced varying results.
While studies show that some have limited remissions without increased mortality, others have actually led to more readmissions and emergency department visitor even an increased risk of death compared to usual care.
Prior to the implementation of these policies, VA hospitals had lower readmission rates and lower mortality rates than non-VA hospitals; however, little was known about the relative performance of VA and non-VA hospitals on COPD readmissions and mortality following their implementation.
“Researchers had previously described differing outcomes for patients hospitalized for heart failure at VA and non-VA hospitals following the implementation of these policies, so we were interested to see how the outcomes compared regarding patients who were hospitalized for COPD,” said Stephanie LaBedz, MD, whose research group at the University of Illinois at Chicago led a new study that provides some answers.1
The study in Chronic Obstructive Pulmonary Diseases used publicly available data from CMS Hospital Compare that tracked hospital-level risk-standardized readmission and mortality rates in both VA and non-VA hospitals. The data included Medicare beneficiaries hospitalized for COPD over a three-year period from July 1, 2015, to June 30, 2018.
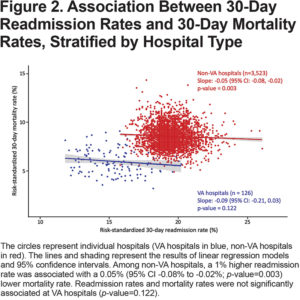
Factors such as patient age, comorbid conditions and indicators of frailty were accounted for in risk-standardized readmission and mortality rates. Non-VA hospitals were further classified according to teaching status, safety-net status, and urban vs. rural location. Associations between hospital-level readmission and mortality rates were evaluated using linear regression models in all hospitals and within VA and non-VA strata.
Key findings were:
- VA hospitals had a lower mean readmission rate — 15.3% (11.8% to 20.2%) at 127 VA hospitals—compared to 19.5% (15.8% to 26.1%) at 3,575 non-VA hospitals.
- VA hospitals had a lower mean risk-standardized 30-day mortality rate — 6.0% at 126 VA hospitals (3.2% to 10.5%) — compared to 8.5% (4.9% to 14.3%) at 3,538 non-VA hospitals.
- Among non-VA hospitals, those classified as non-teaching hospitals, no safety-net hospitals and rural hospitals had significantly lower readmission rates and higher mortality rates compared to teaching hospitals, safety-net hospitals and urban hospitals, respectively.
In sum, VA hospitals outperformed non-VA hospitals from 2015-2018 in COPD readmission rates and COPD mortality rates, LaBedz told U.S. Medicine, adding that possible residual confounding in the CMS risk-adjustment models could make “interpreting these findings a bit more nuanced.” At the hospital level, readmission rates were inversely or negatively associated with mortality rates at non-VA hospitals, meaning that hospitals with lower readmission rates tended to have higher mortality rates, she said.
The authors cited several potential explanations as to why efforts to reduce readmissions might result in different outcomes at VA and non-VA hospitals: the availability of post-hospital transitional care (such as arranging for follow-up appointments), the effects of financial penalties and reimbursement models on resources available to provide high-quality care and differences in data quality or patient populations unaccounted for in the risk-adjustment models.
Some of the limitations of the study are the use of hospital-level data as opposed to more granular patient-level data, the cross-sectional design, and potential selection bias since the CMS-risk adjustment formula for hospital readmission rates does not account for the competing risk of death, LaBedz said.
The authors stated that lack of patient-level data in the study limits the ability to elucidate potential sources of residual confounding, but previous studies have noted differences in coding practices and in social determinants of health among patients served by different hospitals also contribute to variations in risk-adjusted readmission and mortality rates.
Outperforming Non-VA Hospitals
For VA hospitals, the findings provide evidence that policies to lower readmission rates for COPD are working. “VA hospitals appear to be outperforming non-VA hospitals in both COPD readmission rates and COPD mortality rates following the implementation of policies intended to reduce readmissions,” LaBedz explained. “VA hospitals had outperformed non-VA hospitals prior to these policies, but our research suggests the performance gaps may be widening,”
Because of possible residual confounding, however, LaBedz cautioned that the publicly available COPD readmission and mortality rates may not be suitable for direct comparisons between VA and non-VA hospitals. “This is important for veterans who are looking to make informed choices about where to seek healthcare, whether it be within the VA system or outside the VA system, using Hospital Compare data.”
- LaBedz SL, Krishnan JA, Chung YC, et al. Chronic obstructive pulmonary disease outcomes at Veterans Affairs versus non-Veterans Affairs hospitals. Chronic Obstructive Pulmonary Diseases. 2021. Published online May 11, 2021. DOI: https://doi.org/10.15326/jcopdf.2021.0201.