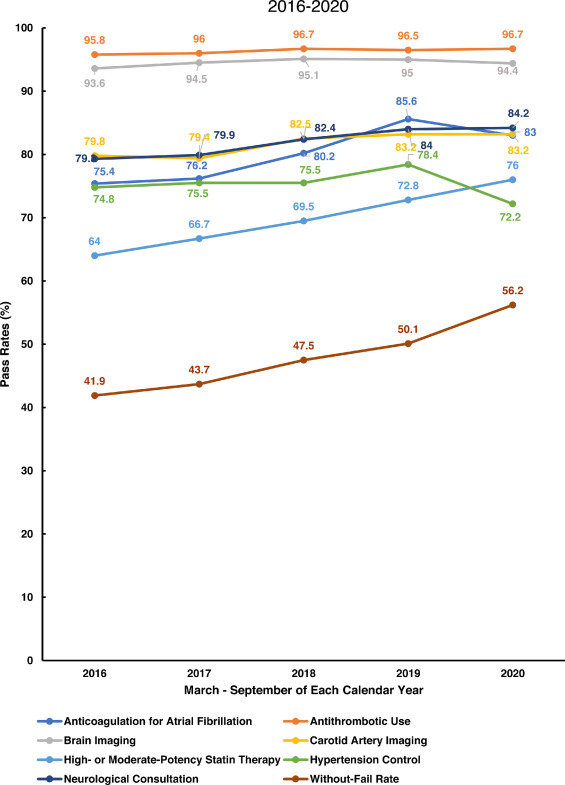
Click to Enlarge: Displays the quality of care for seven processes of care plus the without-fail rate for the period March to September (2016 through 2020). Source: Journal of Stroke and Cardiovascular Disease
The overall quality of care for stroke patients in the nation’s largest healthcare system did not decline during the COVID-19 pandemic, according to a new study.
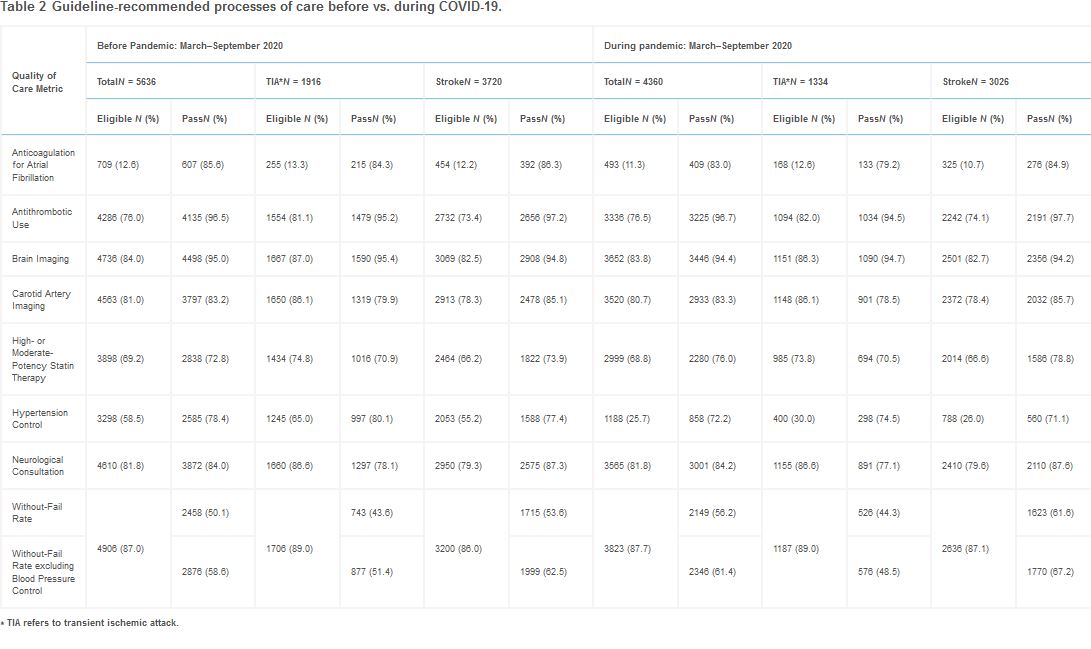
The retrospective cohort study published in the Journal of Stroke & Cerebrovascular Diseases compared the quality of care and outcomes for patients with acute ischemic stroke (AIS) and transient ischemic attack (TIA), often called mini-stroke, before (March–September 2019) vs. during (March-September 2020) the COVID-19 pandemic across VA healthcare system. Secondary analyses examined quality of care during March-September of each year from 2016 through 2018.1
Patients at 128 VA hospitals with an emergency department visit or inpatient stay for stroke and TIA from 2016-2020 were identified based on admission diagnoses. Electronic health record data were used to identify patient characteristics, quality of care and outcomes.
The researchers used an overall measure of quality of care called the “without-fail rate” that was calculated for each patient as either present or absent based on whether the patient received all of the care for which they were eligible among seven processes of care, Dawn Bravata, MD, senior author of the study from the VA’s Health Services Research and Development, Indiana University School of Medicine, the Florey Institute of Neuroscience and Mental Health and Regenstrief Institute, explained in an email.
The seven individual processes of care were:
- Brain imaging,
- Carotid artery imaging,
- Anticoagulation for atrial fibrillation,
- Antithrombotics,
- Receipt of high or moderate potency statins,
- Neurology consultation and
- Hypertension control.
Patients could either or fail the measure for the first six processes of care. For the hypertension control measure, patients without a blood pressure measurement within 90 days of hospital discharge were considered ineligible for the measure.
“Overall quality of care for patients with acute ischemic strokes and transient ischemic attacks did not decline during the COVID-19 pandemic in U.S. Department of Veterans Affairs hospitals,” Bravata told U.S. Medicine. “We found that the overall measure of quality of care (the without-fail rate) actually increased during the pandemic: 50.1% pre-pandemic increased to 56.2% during the early pandemic period, meaning the patients received all of the care for which they were eligible. This increase in the overall quality measure was driven by continued increased use of high or moderate potency statins among veteran patients with stroke. The use of high or moderate potency statins has been increasing consistently each year since 2016.”
During the pandemic, a slightly greater number of patients had a stroke rather than a TIA (69.4% vs. 66%), likely because patients with temporary symptoms may have hesitated to seek medical attention during the pandemic.
Death Rates Unchanged
Death rates of patients suffering from stroke and TIA in VA hospitals were not statistically different after risk adjustment before and after the pandemic.
The study found the number of hospitalizations for stroke and TIA was lower during the COVID-19 pandemic. There were nearly 19% fewer hospitalizations for stroke and about 30% fewer hospitalizations for TIA.
Also, patients who sought care for stroke and TIA had far fewer primary care visits, which delayed or deferred care during the pandemic. Early in the pandemic, many in-person clinic visits were postponed or replaced by telehealth visits. Based on VA policy, blood pressure measurements can only be entered into the electronic health record vital sign package if the blood pressure measurement was observed by VA clinical staff either during in-person visits or video visits. As a result, approximately 40%of stroke patients did not have a blood pressure measurement, while only 10% of stroke patients did not have a blood pressure measurement before the pandemic.
However, the increase in statin use was larger than the reduction in hypertension control among patients (receiving a blood pressure measurement in the 90 days following hospital discharge), so there was an overall net improvement in quality of care, Bravata explained.
Because of the robust relationship between blood pressure and stroke risk, primary care clinicians are urged to prioritize hypertension management among patients with stroke and TIA.
“The key issue to consider when evaluating the change in hypertension control was that there were fewer patients with post-discharge blood pressure measurements, which was probably due to fewer patients having a primary care visit in the 90 days after discharge in 2020 (82.1% versus 51.5% for patients with TIA and 79.8 % versus 52.5% for patients with stroke),” Bravata told U.S. Medicine. “Clinicians and hospital administrators should ensure that patients with stroke and TIA should be prioritized to receive post-discharge primary care to facilitate hypertension management.”
Although there have been other published reports about quality of care for patients with stroke during the pandemic, the national scope of this cohort and the inclusion of both acute processes of care (e.g., brain imaging) and post-discharge care (e.g., hypertension management) is a strength of this work, Bravata wrote.
“The examination of trajectories of quality of care is also a strength of our study and was certainly very helpful in understanding how prescribing of high or moderate potency statins have been changing over time,” Bravata explained.
- Myers LJ, Perkins AJ, Kilkenny MF, Bravata DM. Quality of Care and Outcomes for Patients with Acute Ischemic Stroke and Transient Ischemic Attack During the COVID-19 Pandemic. J Stroke Cerebrovasc Dis. 2022 Jun;31(6):106455. doi: 10.1016/j.jstrokecerebrovasdis.2022.106455. Epub 2022 Apr 5. PMID: 35395471; PMCID: PMC8983051.