GAO Suggests VistA Will Be Around for Next Decade
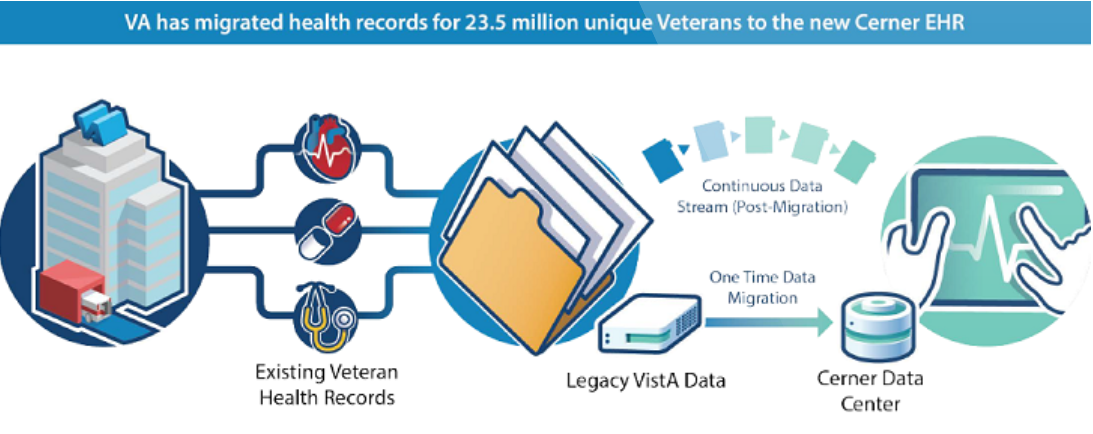
The VA recently celebrated the successful transfer of 23.5 million veterans’ health records to a shared data center with the DoD. This sets the stage for the “go-live” of VA’s EHR solution next year. Graphic from VAntage Point blog.
WASHINGTON — As VA moves forward with the comprehensive overhaul of its electronic health records system, the department will still need to keep its legacy EHR system functioning well into the next decade. A recent Government Accountability Office report suggests, however, that the costs to do that—already totaling in the billions—may have been underestimated.
Furthermore, according to the GAO, VA is unsure, at least for the time being, how deeply entrenched that legacy system is facility-by-facility.
The Veterans Health Information System and Technology Architecture, or VistA, can trace its earliest roots back to the late 1970s when its first modules were launched at VA sites. During its peak in the 1990s and early 2000s, it was considered one of the best EHR systems available, and efforts were even made by members of Congress to get DoD to begin using the system.
Today, VistA is outdated, costly to maintain and does not support the long-sought goal of easy data-sharing with DoD and the private sector. VA has contracted with Cerner, an information technology company, to provide a new EHR that will interact with DoD’s Cerner-created system. The replacement will take place facility by facility over the next decade with the system being piloted at three facilities in the Pacific Northwest starting in March 2020. Because the replacement is happening in stages, VistA will have to be kept functioning at facilities as they wait to receive the Cerner system.
According to the GAO report, VistA’s decadeslong organic growth has resulted in multiple versions of the system, with different facilities customizing it to meet their needs. Consequently, VA has no set definition of what falls under VistA.
“What began as a guerilla IT project has sprawled into a massive decentralized system in an archaic coding language,” declared. Rep. Susie Lee (D-NV), chair of the House VA Subcommittee on Technology Modernization, at a hearing last month. “Within the VA, there are at least 130 versions of VistA across 1,500 sites. No version is the same, and the system connects to various applications and devices through interfaces.”
Individual Facility Surveys
VA will not fully understand how VistA is used at each facility until it conducts individual facility surveys—a built-in part of the rollout process. VA has already conducted surveys at its three pilot sites, and officials are confident the process will yield everything the department needs to know for a successful EHR replacement.
“Part of this learning process is the on-site surveys in anticipation of the Cerner rollout,” explained Paul Tibbits, VA’s director of the Office of Technical Integration. “As they happen, in a very definitive way we’ll understand everything about VistA at that site. As the waves move forward, we’ll become more and more definitive of the cost estimates we have to live with now.”
The current cost estimate is $4.83 billion over the decadelong rollout. This estimate was creating using cost analyses from previous years of VistA upkeep. But the GAO investigators have noted that these analyses are incomplete and poorly documented.
“VA believes VistA has cost $2.3 billion between 2015 and 2017, but this figure is neither reliable nor comprehensive,” explained Carol Harris, GAO’s director of information technology acquisition management. “VA can only reliably account for $1 billion total. The rest was not well documented. VA’s subject matter experts were unclear on how to account for Vista versus nonVista costs.”
Some items were also omitted from the estimated cost, such as additional hosting.
“[VA] is not in a position to report annual costs to develop and sustain VistA,” Harris declared. “The department lacks data to make critical management decisions for sustaining VistA over the next 10 years.”
VA officials recognize that the process of replacing one EHR with another can be a fraught one with the potential to create gaps in service—something they hope to avoid as much as possible.
“The biggest challenges and biggest risks to us are complex clinical scenarios where patients might be migrating across multiple clinical settings or where longitudinal care is critical to clinical decision-making,” explained VA Senior Medical Advisor Thomas O’Toole, MD. “That is something we’re in the process of looking at very closely in the context of the initial operating capabilities to ensure those workflow processes are identified in advance and that clinicians know what to expect.”
One component of VistA that Cerner will not be able to replace is its prosthetics applications. VA’s short-term approach will be to maintain the current prosthetics system and create an interface for until it can be adequately replicated in the new Cerner EHR.

