Most Effective When Combined with Metformin
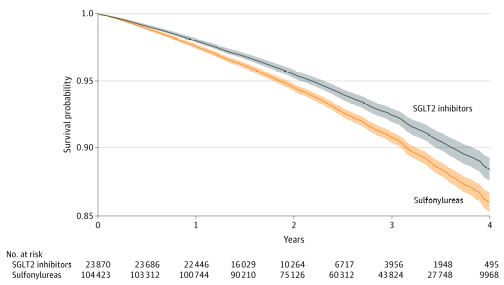
Click to Enlarge: Adjusted Intention-to-Treat Survival Probability for All-Cause MortalitySurvival probability in the sodium-glucose cotransporter 2 (SGLT2) inhibitor and sulfonylurea treatment arms. Shaded bands represent 95% CIs.
ST. LOUIS — Sodium-glucose cotransporter 2 (SGLT2) inhibitors, a relatively new class of antihyperglycemics, have become an important tool in the treatment of Type 2 diabetes—a disease that affects an estimated 25% of VA patients.1
Benefits of the drugs in clinical studies have included glucose control, weight loss, blood pressure reduction and decreased risk of cardiovascular events. 2 Randomized clinical trials examining the effects of SGLT2 inhibitors have compared them only to placebo, however. Head-to-head comparisons with older second-line antihyperglycemic agents—specifically sulfonylureas—as well as studies of SGLT2 as a monotherapy have been lacking.
A new study led by researchers at the VA St Louis Health Care System confirms the benefits of SGLT2 inhibitors over sulfonylureas and demonstrates the importance of using them in addition to—rather than as a replacement—for the standard first-line treatment metformin. 3
The cohort study utilized VA data to compare the use of SGLT2 inhibitors vs sulfonylureas in patients receiving metformin for treatment of Type 2 diabetes. Among the 128, 293 participants (mean [SD] age, 64.60 [9.84] years; 122,096 [95.17%] men), 23,870 received an SGLT2 inhibitor, and 104,423 received a sulfonylurea.
Key findings of the study included:
- Compared with sulfonylureas, SGLT2 inhibitors were associated with reduced risk of all-cause mortality (hazard ratio [HR], 0.81; 95% CI, 0.75-0.87), yielding an event rate difference of -5.15 (95% CI, -7.16 to -3.02) deaths per 1,000 person-years.
- Compared with sulfonylureas, SGLT2 inhibitors were associated with a reduced risk of death, regardless of cardiovascular disease status, in several categories of estimated glomerular filtration rate (including rates from >90 to ≤30 mL/min/1.73 m2) and in participants with no albuminuria (albumin to creatinine ratio [ACR] ≤30 mg/g), microalbuminuria (ACR >30 to ≤300 mg/g) and macroalbuminuria (ACR >300 mg/g).
- Continued use of SGLT2 inhibitors was associated with a reduced risk of death compared with continued use of sulfonylureas in per-protocol analyses, (HR, 0.66; 95% CI, 0.60-0.74; event rate difference, -10.10; 95% CI, -12.97 to -7.24 deaths per 1,000 person-years).
Further, multiple subgroup analyses were conducted in predefined subgroups based on:
- Those younger and older than 65 years,
- Baseline cardiovascular disease status,
- eGFR status (≥90, <90 to ≥60, <60 to ≥45, and <45 mL/min/1.73 m2),
- Albuminuria status,
- BMI categories (≤25, 25-≤30, and >30), and
- Use of medications, including insulin, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers and diuretics.
In all subgroups, SGLT2 inhibitors “came out on top,” lead author Ziyad Al-Aly, MD, told U.S. Medicine.
“The study showed very clearly that SGLT2 inhibitors work better at reducing all-cause mortality,” Ziyad Al-Aly, MD, director of the Clinical Epidemiology Center and the chief of Research and Education Service at Veterans Affairs St. Louis Health Care System, told U.S. Medicine. “It was good to see that our hunch was confirmed in real-world data, that the newer SGLT2 inhibitors are working better than the drugs we have been using for 30 years.”
Adding SGLT2 Inhibitors to Metformin
The benefits of SGLT2 inhibitors are greatest when the drugs are added to metformin, the study showed. In additional per-protocol analyses, continued use of SGLT2 inhibitors with metformin was associated with a reduced risk of death compared with SGLT2 inhibitor treatment without metformin (HR, 0.70; 95% CI, 0.50-0.97; event rate difference, -7.62; 95% CI, -17.12 to -0.48 deaths per 1,000 person-years).
Al-Aly said this finding is important for clinicians who might consider bypassing metformin and prescribing SGLT2 as a monotherapy. “The evidence and the guideline are that SGLT2s are second line—they are added to metformin. Yet some clinicians are bypassing metformin and going straight to SGLT2 inhibitors,” he said. “We wanted to know if metformin was adding anything or contributing to risk reduction, so we evaluated people who are on SGLT2 inhibitors and metformin compared to people on SGLT2 inhibitors without metformin. The people without metformin were not benefiting as much, so the combination of SGLT2 and metformin was better than SGLT2 alone.”
What the study didn’t do was to compare SGLT2 alone to metformin alone. Because of metformin’s long-standing safety record, tolerability and beneficial metabolic profile, Al-Aly said he suspects it will continue to be the preferred choice as a first-line treatment for Type 2 diabetes. He said head-to-head studies comparing SGLT2 inhibitors to metformin are needed before SGLT2 inhibitors can be recommended as a first-line treatment.
As a second-line treatment, the results provide real-world evidence on the association of SGLT2 inhibitor use with the risk of all-cause death, the study’s authors concluded. “The results may help guide the choice of antihyperglycemic therapy in people with Type 2 diabetes.”
- Liu Y, Sayam S, Shao X, et al. Prevalence of and Trends in Diabetes Among Veterans, United States, 2005–2014. Preventing Chronic Disease. Published online December 14, 2017. DOI: 10.5888/pcd14.170230.
- Hsia DS, Grove O, Cefalu WT. An Update on SGLT2 Inhibitors for the Treatment of Diabetes Mellitus. Current Opinion in Endocrinology, Diabetes and Obesity. 2017; 24 (1): 73-79. DOI: 10.1097/MED.0000000000000311.
- Xie Y, Bowe G, Gibson AK, et al. Comparative Effectiveness of Sodium-Glucose Cotransporter 2 Inhibitors vs Sulfonylureas in Patients With Type 2 Diabetes. JAMA Internal Medicine. Published online June 28, 2021. DOI:10.1001/jamainternmed.2021.2488.

