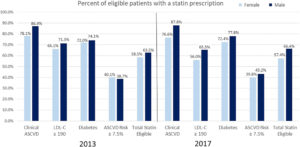
Statin use prevalence by ACC/AHA eligibility categories in 2013 and 2017, by sex. ACC/AHA, American College of Cardiology/American Heart Association; ASCVD, atherosclerotic cardiovascular disease; LDL‐C, low‐density lipoprotein cholesterol
COLUMBIA, SC — In 2013, the American College of Cardiology and American Heart Association issued updated guidelines significantly expanding the number of patients who should be considered candidates for statin therapy. Subsequent years have not seen the expected increase in statin use, with some populations at high risk for heart disease, including those with human immunodeficiency virus and chronic hepatitis C virus infection, seldom prescribed the common drugs.
From 2002 to 2013, the use of statins rose nearly 80%, increasing from 21.8 million individuals to 39.2 million people in the U.S. 1 Since then, the percentage of Americans prescribed the low-density lipoprotein-reducing drugs has largely leveled off. A recent study of a large health system found that 62% of eligible patients were prescribed statins in 2017, up only slightly from the 61% seen in 2013. 2
“We wanted to do the study, given that national estimates show full implementation of the guidelines would have significant potential to help save lives,” said lead author Abbey Sidebottom, principal research scientist at Minneapolis-based Allina Health. “It’s estimated that, by treating all statin-eligible adults who are currently untreated, we could prevent more than 240,000 atherosclerotic cardiovascular disease (ASCVD) events every year in the U.S., which include coronary heart disease, cardiovascular deaths, and fatal and nonfatal strokes.”
For the VA, minimizing the risk of cardiovascular morbidity and mortality for veterans with HCV and HIV is a priority. The VA cares for more patients infected with HCV or HIV or co-infected with both viruses than any other healthcare system in the country. The development of antiretroviral therapy (ART) for HIV shifted the focus of VA providers from short-term survival to longer-term issues such as cardioprotective behaviors and therapies. At the same time, the VA’s success in curing more than 100,000 veterans of HCV infections with direct-acting antivirals increased the attention paid to heart disease in patients who have or have had HCV.
In this environment, it would appear that prescribing statins, which are associated with a reduction in cardiovascular events, would be standard for veterans with HCV or HIV. But it isn’t. Some studies have linked statins with increased liver enzyme abnormalities, making many providers a little nervous about using them in patients with HCV or HCV/HIV co-infection, who often already have some degree of liver injury.
Researchers at the Dorn Research Institute of the W.J.B. Dorn VAMC and the University of South Carolina, both in Columbia, sought to determine whether statins increased the risk of liver injury in veterans with HCV or HIV by analyzing data from the Veterans Affairs Informatics and Comp,uting Infrastructure (VINCI) database. 3
What the study led by S. Scott Sutton, PharmD, found across a large group of veterans directly countered concerns about liver damage.
The team retrospectively analyzed the records of 166,439 veterans, including those with HIV and/or HCV as well as uninfected veterans, who were followed for 18 months from index date. All patients had filled at least one prescription for any drug during the baseline period, had a Fibrosis-4 Index score during baseline, and had at least one AST or ALT laboratory result during follow-up.
Continue Reading this Article: Acute Liver Injury
