COVID-19 Is Significantly Increasing Remote Care
WASHINGTON — When the VA recently received $17.2 billion in funding from the CARES Act, one of the priorities was providing telehealth resources for veterans seeking in-home care.
That is critical, the agency said, because it sought to treat veterans with manageable symptoms remotely to avoid overwhelming VHA facilities and to prevent exposure to novel coronavirus patients. Telehealth also is essential to providing mental health counseling for veterans with post-traumatic stress disorder and other conditions exacerbated by the stress of the global COVID-19 pandemic.
In fiscal year 2019, VA provided 2.6 million telehealth episodes of care to more than 900,000 veterans, representing a 16% increase from the previous year. The CARES Act provided additional funding so that nonessential VA employees could work at home and care for more veterans remotely; the agency requested funds to purchase at least 180,000 new devices.
An issue lost in the rush to continue VA operations in the age of COVID-19 is how veterans feel about telehealth care. A recent study in the Journal of Medical Internet Research addressed that issue, although the survey was conducted well before the novel coronavirus outbreak.1
Four years ago, the VA’s Offices of Rural Health and Connected Care developed a pilot initiative and began to distribute video-enabled tablets to veterans who did not have the necessary technology and who had a geographic, clinical or social barrier to in-person health care access. For the recent study, a survey conducted by VA Affairs Palo Alto, CA, Health Care System researchers determined that 32.1% of 604 veterans who had received tablet devices indicated that they would prefer to conduct their future VA appointments by video, 31.8% indicated that they would prefer these visits in person, and 35.7% indicated their preference was “about the same.”
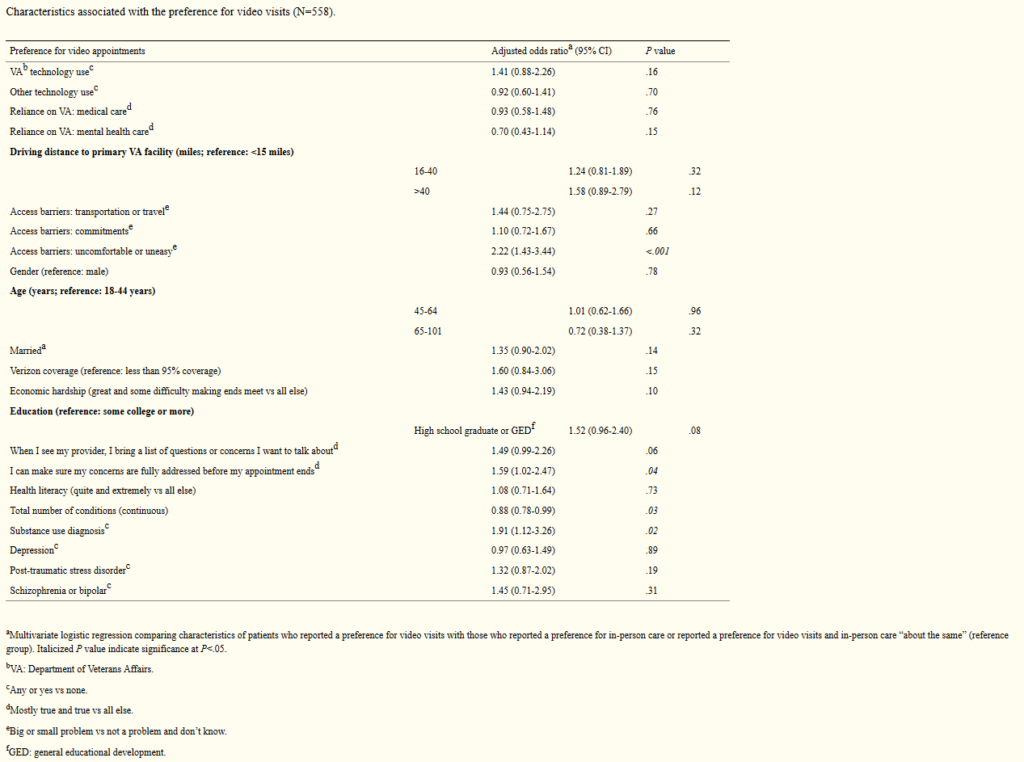
Analysis by the researchers concluded that patients were more likely to report a preference for video-based care if they reported the barrier of feeling uncomfortable or uneasy in the VA setting (adjusted odds ratio [AOR] 2.22, 95% CI 0.88-2.26; P<.001), if they indicated mostly/very true to the statement “I can make sure my concerns are fully addressed before my appointment ends” (AOR 1.59, 95% CI 1.02-2.47; P=.04), or if they had a substance use disorder in the year before receiving the tablet (AOR 1.91, 95% CI 1.12-3.26; P=.02).
On the other hand, veterans were less likely to prefer video-based care if they had a greater number of chronic conditions (AOR 0.88, 95% CI 0.78-0.99; P=.03). The authors also pointed to trends suggesting that patients were also more likely to prefer video-based care if they had less than college education (AOR 1.52, 95% CI 0.96-2.40; P=.08) and if they indicated mostly/very true to the question “When I see my doctor, I bring a list of questions or concerns I want to talk about” (AOR 1.49, 95% CI 0.99-2.26; P=.06).
“Technology is playing an increasingly important role in enhancing health care access and delivery for patients, especially for those who are geographically isolated or homebound,” the researchers explained. “Although VA has evolved to become both a provider and payer of care, its priority of ensuring access to high-quality care for veterans has not changed. The 2018 Mission Act further expands the role of telemedicine in the VA, including the approved use of video visits in the home and across state lines.”
Yet, they add, “Critical issues remain owing to variations in broadband infrastructure that will influence the adoption and use of these technologies. This study provides important information about patient experiences with VA-issued tablets and their preferences for video versus in-person care. The findings may inform the development of assessment and training tools to improve patient targeting and support for tablet recipients as well as opportunities to improve engagement in video visits.”
Over a two-year pilot period, 5,000 tablets were distributed to 6745 patients at 86 (out of 130) VA healthcare systems in all 18 geographic regions of the VA’s health care network. About half of the tablet recipients lived in rural areas and 75% had a mental illness diagnosis.
The report noted that tablets were predominantly used for mental health care, as well as for spinal cord injury care, primary care, palliative care, rehabilitation and other services.
The 764 VA patients responding to the survey were more likely to be younger than 65, be non-Hispanic blacks, live in an urban area, have a greater number of mental health conditions and to make use of the tablet.
Respondents revealed that their most common barriers to care were travel time (503/757, 66.4%), travel cost (416/753, 55.2%), health conditions (405/754, 53.7%), bad weather (426/754, 56.5%) and feeling uncomfortable or uneasy at the VA (248/753, 32.9%). The factor analysis created three categories of barriers from the original list: transportation, outside commitment—such as work, school and caregiving responsibilities—and a single barrier related to feeling uncomfortable or uneasy at the VA.
Here are some of the veteran comments included in the report, divided by category:
Opportunity to overcome access barriers:
-
“Being handicapped & having no transportation, I have to make special arrangements for transportation & pack a lunch for my wife & myself.”
-
“Sometimes it’s nice to have a face-to-face visit with my psychologist, and sometimes it’s nice not to have to drive 50 miles one way.”
-
“I would prefer video, because it would expose me less to sick people. This benefits me a lot being a transplant recipient. And my caregiver wouldn’t have to take off work to take me to the doctor.”
Perceptions of quality of care provided by video visits versus in-person care:
-
“I get to see the provider just as if I came to VA in person so to me that is about the same or just as good.”
-
“The care that I receive is the same in person or by video, excellent”
Feasibility of receiving necessary care by video visits vs. in-person:
-
“Sometimes doctors need to examine patients. I think it’s wonderful for therapy, because all I need to do is talk.”
-
“I prefer a video chat with mental health provider rather than the 2.5-hour commute for a short session. I like to see my medical doctor and orthopedic doctor in person. Video visits are a good way to have questions answered.”
Technological issues:
-
“Need to give a class on how to use the tablet and make sure the connection & passwords are done right.”
-
“Dropping video/calls; it’s no longer used because of our location”
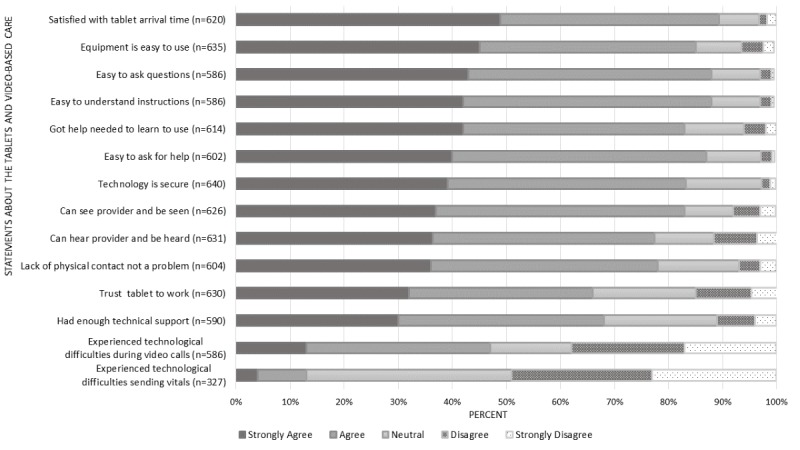
“The strong satisfaction ratings for tablets and the fact that characteristics such as age, income, health literacy, distance from the closest VA facility, and prior technology use were not significantly associated with tablet preference suggest that engagement in video-based care is possible for many types of patients, including those who are often considered part of the digital divide (i.e., individuals who are older, have a low income, and have greater health or disability challenges),” the authors wrote.
They added that, by providing tablets to that population, the VA has been able to engage veterans who might otherwise be left behind in technology-focused initiatives.
Researchers also pointed out the importance of the link between patients’ communication style and preference for video visits. “The results indicate the importance of identifying patients who are amenable to using technology for their care and identifying opportunities to improve training for patients and providers who want to conduct video visits,” they added.
The study emphasized that, even patients who initially decline telehealth often end up being satisfied with it, noting, “Despite the technical challenges that may hinder initial use, once patients participate in a video visit, they often perceive it to be of the same or better quality than in-person care. However, patients acknowledge that video visits cannot fully replace in-person care, particularly when physical examinations are needed for decision-making.”
-
Slightam C, Gregory AJ, Hu J, et al. Patient Perceptions of Video Visits Using Veterans Affairs Telehealth Tablets: Survey Study. J Med Internet Res. 2020;22(4):e15682. Published 2020 Apr 15. doi:10.2196/15682