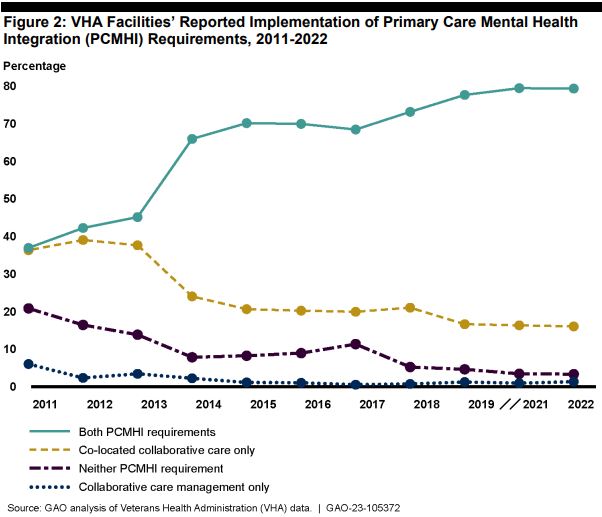
Click to Enlarge: VHA facilities serving at least 5,000 unique veterans annually are required to provide both colocated collaborative care and collaborative care management. For co-located collaborative care, facilities must make mental health providers available within primary care settings to assess and treat veterans with mental health symptoms and conditions. For collaborative care management, facilities must follow up with those veterans to monitor symptoms and adherence to and any side effects of medication and provide education and referral services. The number of VHA facilities required to provide these PCMHI services may vary depending on whether they serve at least 5,000 unique veterans annually. For example, in 2011, 336 facilities were required to have both co-located collaborative care and collaborative care management. That number increased every year over the following decade and, as of the 2022 annual survey, had increased to 455 facilities. According to VHA’s Office of Mental Health and Suicide Prevention (OMHSP) officials, certain VHA facilities have been required to complete an annual PCMHI survey since 2011. However, they did not administer the 2020 annual survey because of the COVID-19 pandemic. According to OMHSP, these surveys serve as a point-in-time assessment that captures services that VHA facilities provide as of a certain date. For example, the date for the 2022 annual survey was February 1, 2022.
WASHINGTON, DC — For years, VA has been working to integrate mental healthcare into primary care and requires facilities serving at least 5,000 veterans annually to have a mental health provider available within primary care settings.
These psychologists, psychiatrists and social workers are there to work collaboratively and share responsibility with primary care providers to assess and treat veterans. However, staffing difficulties have slowed this effort, and a recent report from the Government Accountability Office (GAO) found that 21% of VA facilities still do not have these mental healthcare providers available as an integrated part of the care team.
According to VA, the number of veterans receiving mental healthcare rose by 85% between 2006 and 2020, and VA projects that the demand for outpatient mental health services will continue to grow by about 32% over the next decade. In 2007, VA began implementing a Primary Care Mental Health Integration (PCMHI) model to increase the quality and access of mental healthcare across the department and to free up mental health specialty settings to focus on severe mental illnesses.
The department has found that not only does having mental health providers available during primary care appointments speed up diagnoses, but veterans also are more receptive to mental health treatment in that setting.
Because PCMHI providers are required to have relatively flexible schedules, allowing them to be on-call to meet with veterans who come in for primary care appointments, they need to be dedicated staff. Many VA facilities, even those that have met the integration requirements, find this a challenge.
According to annual survey results conducted from 2013 to 2022, between 54% and 65% of VA facilities reported their PCMHI programs were not adequately staffed, based on needed services that year. In 2022, 43% of facilities pointed to staffing challenges as their No. 1 concern, driven in large part by a spike in PCMHI staff leaving over the previous two years.
In addition to staff turnover, facility leaders blamed the national shortage of mental health providers, as well as salary discrepancies between VA and the private sector, provider preferences to deliver care virtually and the department’s “slow and complicated” hiring process.
“VA medical center officials told us that staffing challenges can affect all PCMHI positions, but some positions are more difficult to fill than others,” GAO officials noted in their report. “For example, officials from one VA medical center said that psychologist positions are especially difficult to fill because their VA medical center does not offer psychologists salaries that are competitive with the private sector, or other incentives such as retention or relocation bonus or Education Debt Reduction Program benefits.”
At another facility, officials told the researchers that psychiatrists in that area can earn twice as much in the private sector compared to VA.
Facilities failing to meet the integration goals are exploring mitigation strategies to use as workarounds for staffing challenges. Two facilities are offering hybrid positions, in which PCMHI providers can work a combination of in-person and virtual hours. One medical center official said she is looking at ways to reduce the amount of unnecessary administrative tasks by offering additional support or technology, since providers complain about this aspect of their workload most often.
Another VA medical center has temporarily reassigned a person who was working on another unit to PCMHI duties, training that person to help provide more coverage.
On the national level, the Office of Mental Health and Suicide Prevention (OMHSP) said they provided guidance to VISNs and VA facilities to help them develop local staffing priorities and allocations. However, they have not developed a plan to mitigate staffing challenges nationally, since staffing decisions are determined at the local and VISN level. They also have not created any monitoring plan to track improvement in those facilities who are struggling or to determine whether the various mitigation strategies some are using are proving effective.
GAO researchers said that, if VA wants more facilities to meet its PCMHI goals, the department should more formally track the staffing at these struggling facilities so that it can know when and how to provide support.
“A full complement of mental health professionals is imperative for VA to be able to meet the rapid growth in demand for VA mental health services,” the report concludes. “The expected continued growth in demand for mental health services may only exacerbate long-standing and persistent PCMHI-related staffing challenges.”
- Government Accountability Office Report to Congress: Veterans Healthcare Staffing Challenges Persist for Fully Integrating Mental Health and Primary Care Services. December 2022

