PHILADELPHIA — Caring for prostate cancer patients often involves much more than managing the urological symptoms. Research increasingly shows that mental health can affect how well those men respond to treatment.
A recent study discussed how depression is common after a diagnosis of prostate cancer and how the condition can contribute to poor outcomes, especially among African American patients.
The authors from the Corporal Michael J. Crescenz VAMC, the VA Center for Health Equity Research and Promotion and the Perelman School of Medicine at the University of Pennsylvania, all in Philadelphia, sought to assess the incidence and management of depression and its impact on overall mortality among African American and white veterans with localized prostate cancer.
To do that, the authors used the VHA Corporate Data Warehouse to identify 40,412 African American and non-Hispanic white men diagnosed with localized prostate cancer from 2001 to 2013. They followed the patients through 2019.
Participants had a median age of 67 years, and about one-fourth of them were African American.
As part of the analysis, published in the journal Cancer, researchers looked at associations between race and incident depression and sought to identify disparities. Related research also was accepted and made available at the 2021 ASCO Annual Meeting.1
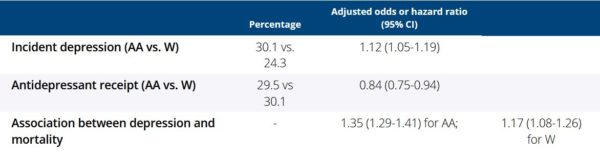
Results indicated that nearly a fourth, 24.5%, were diagnosed with depression after a prostate cancer diagnosis and that incident depression was associated with higher all-cause mortality (adjusted hazard ratio [aHR], 1.27; 95% confidence interval [CI], 1.23-1.32). The authors pointed out that the hazard of all-cause mortality associated with depression was greater for African American veterans than white veterans (aHR, 1.32 [95% CI, 1.26-1.38] vs 1.15 [95% CI, 1.07-1.24]; race-by-depression interaction P < 0.001).
While African American veterans were more likely than white veterans to be diagnosed with depression (29.3% vs 23.2%; adjusted odds ratio [aOR], 1.15; 95% CI, 1.09-1.21), they were slightly less likely to be prescribed an antidepressant (30.4% vs. 31.7%; aOR, 0.85; 95% CI, 0.77-0.93), researchers from the same VAMC reported at the recent 2021 American Society of Clinical Oncology (ASCO) annual meeting.2
Furthermore, analyses indicated that hazard ratio of all-cause mortality associated with depression among African Americans was significantly greater than that of white veterans, although being prescribed an antidepressant was not associated with improved mortality (aHR 1.05 [95% CI 0.97-1.13]), which was not moderated by race.
“Depression was common among men with prostate cancer within a large equal-access health care system, and African American men had more adverse depression-related outcomes than white men,” the authors wrote. “Identifying and managing incident depression should be a key target of efforts to improve prostate cancer outcomes and disparities.”
Mental health concerns with prostate cancer go far beyond depression diagnoses, however. Research looking at a range of cancer diagnoses suggested that adverse mental health effects on patients could, in some cases, lead to suicidal behavior. That is especially of concern to the VA, because suicide rates among veterans are 50% greater than for nonveteran U.S. adults.
The study, also from ASCO 2021, emphasized the importance of understanding associations between cancer and suicide risk among veterans receiving VA healthcare from the VHA.3
A team from the Ann Arbor, MI, VAMC, the Philadelphia VAMC and Duke University assessed associations between new cancer diagnoses and suicide among veterans receiving care from the VHA care. The goal was to identify high-risk diagnostic subgroups and risk periods.
The cohort study identified 4.9 million veterans with VHA use in 2011 and either 2012 or 2013 and without a VHA cancer diagnosis in 2011. They then looked at incident cancer diagnoses, assessed between first VHA use in 2012-2013 and 12/31/2018, grouping them by subtype and stage using VHA Oncology raw data. Information from the VA/DoD Mortality Data Repository identified the date and cause of death for those veterans.
The study calculated crude suicide rates following a new cancer diagnosis for 240,410 veterans from 2012 to 2018. Mortality rates were assessed up to 84 months following diagnosis. On average, however, veteran VHA users were followed for 6.0 years after their first VHA use in 2012-2013 and 2.7 years following a new cancer diagnosis.
Results indicated that a new cancer diagnosis corresponded to a 43% (Adjusted Hazard Ratio [AHR] = 1.43, 95% CI: 1.29, 1.58) higher suicide risk, adjusting for covariates.
Researchers reported that the cancer subtype associated with the highest suicide risk was esophageal cancer (AHR = 5.93, 95% CI: 4.05, 10.51). Other significant subtypes included: head and neck (AHR = 3.44, 95% CI: 2.65, 4.46) and lung cancer (AHR = 2.28, 95% CI: 1.79, 2.90).
Researchers advised that cancer Stages 3 (AHR = 2.29, 95% CI: 1.75, 3.01) and 4 (AHR = 3.45, 95% CI: 2.75, 4.34) at diagnosis were also positively associated with suicide risk. They found that suicide rates were highest in the first three months following a diagnosis (Rate = 128.3 per 100,000 person-years, 95% CI: 100.4, 161.6) but remained elevated through the first year.
- Parikh RB, Gallo JJ, Wong YN, Robinson KW, Cashy JP, Narayan V, Jayadevappa R, Chhatre S. Long-term depression incidence and associated mortality among African American and White prostate cancer survivors. Cancer. 2021 Jun 1. doi: 10.1002/cncr.33656. Epub ahead of print. PMID: 34061986.
- Parikh RB, Gallo JJ, Cashy J, Robinson KW, et. Al. (June 4-8, 2021) Racial disparities in depression incidence, management, and mortality after prostate cancer diagnosis. ASCO 2021 annual meeting. Virtual. https://meetinglibrary.asco.org/record/194952/abstract
- KR, Szymanski BR, Kelley MJ, Katz I, et. Al. . (June 4-8, 2021) Suicide risk following a new cancer diagnosis among veterans in Veterans Health Administration care. ASCO 2021 annual meeting. Virtual. https://meetinglibrary.asco.org/record/200371/abstract