Most Common Solid Tumor Malignancy Among Veterans
NEW YORK — Over the past decade, how prostate cancer is detected and treated at VA healthcare facilities has changed gradually but significantly.
And that has had a consequential effect on patients treated in the system. The VA reports that more than 16,000 veterans are diagnosed each year with prostate cancer, making it the most common solid tumor cancer among its patients.
More statistics have become available recently on prostate cancer in veterans. Through a novel partnership between the Prostate Cancer Foundation and VHA, a curated prostate cancer database was developed with the initial goal of identifying all patients with metastatic disease.1
Results using Natural Language Processing were that 488,984 VHA patients were living with prostate cancer, as of 2019, and that 16,282 of them had metastatic prostate cancer.
As the country’s largest integrated health care system, VHA “captures about 6% of all prostate cancer patients in the entire country,” said Stephen Freedland, MD, director of the Center for Integrative Research in Cancer and Lifestyle, professor of urology at Cedars-Sinai in Los Angeles, and staff physician at the Durham, NC, VAMC in a recent video discussion.
Many factors fuel the high rate of prostate cancer among patients who receive care through the VA. Among them is that prostate cancer prevalence increases with age—with 50% to 60% of men over age 80 having indicative tumors on autopsy—and VA patients are much more likely to be older and male than those in community healthcare systems. Another key reason is that prostate cancer is a presumptive condition for veterans exposed to Agent Orange.
Millions of servicemembers were exposed to Agent Orange, especially in the Vietnam region, and “the men who were exposed to Agent Orange and other battlefield chemicals often present with more aggressive prostate cancer,” Jeffrey Jones, MD, chief of urology at the Michael E. DeBakey VAMC in Houston explained in an article on the PCF website.
“The MEDVAMC is one of the largest primary and tertiary care centers for veterans,” Jones advised. “We treat hundreds of men with localized and metastatic prostate cancer every year.” Of these, between 5 and 10 percent have been exposed to battlefield chemicals such as Agent Orange.”
Agent Orange Exposure
A recent study in Clinical Genitourinary Cancer confirmed that Agent Orange-exposed veterans present at a younger age and higher clinical stages than those who were not exposed to the chemical. Still, concluded the authors from Washington University in St. Louis and the University of Utah in Salt Lake City, little difference was detected in oncologic outcomes after treatment.2
Those researchers also suggested an additional reason for higher mortality rates in veterans with prostate cancer, writing, “Cigarette smoking was associated with a 2- to 3-fold increased risk of death over those who quit or never smoked.” The national Centers for Disease Control and Prevention has noted that about 3 in 10 veterans use tobacco products.
Because prostate cancer and potentially more serious outcomes are so prevalent at the VA, it has had to be at the forefront in advances in care for the disease. A recent study, for example, looked at how the 2012 U.S. Preventive Services Task Force recommendation against the prostate specific antigen screening for prostate cancer affected practice.
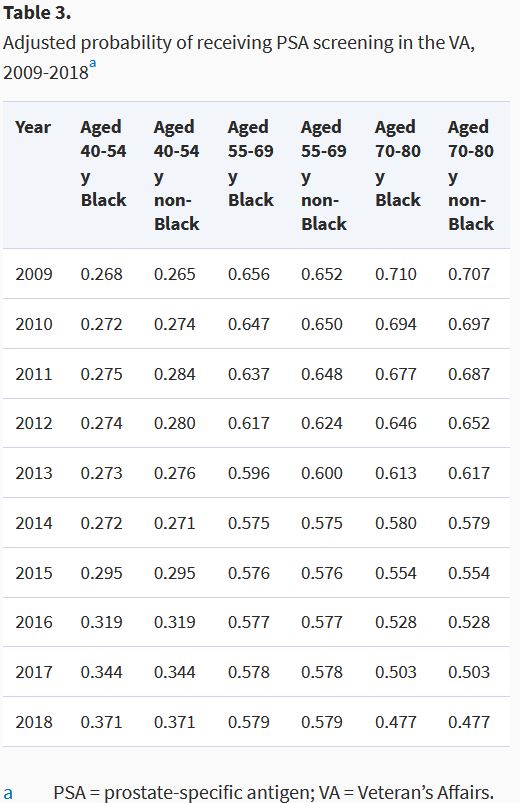
The report in the Journal of the National Cancer Institute looked at PSA screening trends in the VHA before and after the USPSTF recommendation, also seeking to determine if PSA screening was more likely to be ordered based on a veteran’s race or age.3
Researchers used the VA Corporate Data Warehouse to create 10 annual groups of PSA-eligible men covering 2009-2018, identifying all PSA tests performed in the VHA to determine yearly rates of PSA screening.
Results indicated that the overall rate of PSA testing in the VA decreased from 63.3% in 2009 to 51.2% in 2018. The study team pointed out that PSA screening rates also varied significantly by age group during the study period, with men age 70-80 having the highest initial rate and greatest decline (70.6% in 2009 to 48.4% in 2018, p< 0.001). A smaller decline was documented in men age 55-69 (65.2% in 2009 to 58.9% in 2018, p< 0.001) while the youngest cohort, age 40-54, had an increase in PSA screening (26.2% in 2009 to 37.8 in 2018, p< 0.001).
“In this analysis of PSA screening rates among veterans before and after the 2012 USPSTF recommendation against screening, we found that overall PSA screening decreased only modestly, continuing for more than half of the men in our study,” the authors concluded. “Veterans of different races had similar screening rates, suggesting that VA care may minimize racial disparities. Veterans of varying age experienced significantly different trends in PSA screening.”
More changes are on the way. The goal of the PCF partnership was to increase the number of prostate cancer researchers and studies at the VA, boost the number of VA facilities and veterans participating in prostate cancer-related precision medicine and clinical trials and expand access to the wealth of anonymized patient data available through the VA to deepen understanding of the impact of individual genetic variability on the occurrence, progression and treatment of cancer.
“We are building a state-of-the-art oncology program so that veterans with prostate cancer can receive care in the VA equivalent to that in the nation’s leading cancers, regardless of their location,” said Kenute Myrie, PhD, scientific program manager of oncology, VA Office of Research and Development.
- Shelton JB, Lynch J, Alba P, Anglin-Foot T, et. Al. Establishing a Prostate Cancer Data Core in VHA: Early Results. Presented at the Prostate Cancer Foundation 26th Annual Scientific Retreat. Oct. 24-26, 2019. Carlsbad, California.
- Tward AE, Tward JD. The Stage at Presentation and Oncologic Outcomes for Agent Orange Exposed and Non-Exposed United States Veterans Diagnosed With Prostate Cancer. Clin Genitourin Cancer. 2021 Feb 18:S1558-7673(21)00033-1. doi: 10.1016/j.clgc.2021.01.010. Epub ahead of print. PMID: 33731274.
- Becker DJ, Rude T, Walter D, Wang C, et al. The Association of Veterans’ PSA Screening Rates with Changes in USPSTF Recommendations. J Natl Cancer Inst. 2020 Aug 14:djaa120. doi: 10.1093/jnci/djaa120. Epub ahead of print. PMID: 32797212.