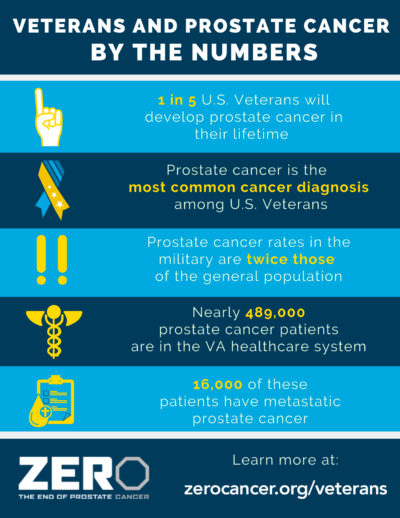
 MINNEAPOLIS — The 15,000 veterans who will be diagnosed with prostate cancer in 2021 have access to more and better treatments than ever. The rapidly expanding arsenal of therapies available to treat the most common cancer in veterans offers good news to the nearly half a million of their fellow former servicemembers receiving care for previously diagnosed prostate cancer through the VA, many of whom are likely to face a recurrence or progression.
MINNEAPOLIS — The 15,000 veterans who will be diagnosed with prostate cancer in 2021 have access to more and better treatments than ever. The rapidly expanding arsenal of therapies available to treat the most common cancer in veterans offers good news to the nearly half a million of their fellow former servicemembers receiving care for previously diagnosed prostate cancer through the VA, many of whom are likely to face a recurrence or progression.
While 90% of men with a prostate cancer diagnosis will die with the disease, not from it, a substantial number of the remaining 10% will experience a far less indolent form of the malignancy that requires aggressive treatment. Matching each veteran with the right treatment for them is a primary goal of the VA.
Watchful waiting vs surgery or radiation
For those with slower growing, localized cancers, regular monitoring with prostate specific antigen (PSA) tests or “watchful waiting” may be the best course of care. A meta-analysis of 67 studies conducted by researchers at the Minneapolis VA Healthcare System found that “active monitoring results in little to no mortality difference vs. radical prostatectomy or external beam radiation plus androgen deprivation,” the most common therapies for localized prostate cancer. The study noted that other treatments lacked sufficient data for analysis.1
Watchful waiting is likely best for men with malignancies detected through PSA testing. For those with clinically detected cancers, the team found that radical prostatectomy reduces mortality compared to radical prostatectomy, but also increases the risk of urinary and erectile dysfunction, two common side effects with significant impact on quality of life.
The effectiveness of surgery may be limited to younger men and those who have intermediate risk disease, the researchers found. For men who have a high risk of progression, external beam radiotherapy, brachytherapy and cryotherapy are also options.
 The findings of the VA study and other research over the last decade has increased awareness of the risk of unnecessary surgery and radiation. “There is a need to reduce the burden to patients of overtreatment if the prostate cancer is slow growing,” said Daniel Suzman, MD, a medical oncologist in the FDA’s Office of Oncologic Diseases in the Center for Drug Evaluation and Research. To reduce that risk, the U.S. Preventative Services Task Force recommends against PSA-based testing in men over age 70, who have relatively low risk of developing symptomatic prostate cancer and a high risk of side effects from treatment.
The findings of the VA study and other research over the last decade has increased awareness of the risk of unnecessary surgery and radiation. “There is a need to reduce the burden to patients of overtreatment if the prostate cancer is slow growing,” said Daniel Suzman, MD, a medical oncologist in the FDA’s Office of Oncologic Diseases in the Center for Drug Evaluation and Research. To reduce that risk, the U.S. Preventative Services Task Force recommends against PSA-based testing in men over age 70, who have relatively low risk of developing symptomatic prostate cancer and a high risk of side effects from treatment.
“I hope that clinical guidelines incorporate this information and find a broader role for watchful waiting and PSA-based testing for most men,” said the study’s lead researcher, Timothy Wilt, MD, of Minneapolis VA Center for Care Delivery and Outcomes Research, and the Minnesota Agency for Healthcare Research and Quality Evidence-based Practice Center.
Hormone therapy
Some men have hormone therapy along with radiation therapy to treat localized or regional prostate cancer. Also called androgen deprivation therapy (ADT), it is also frequently used to treat prostate cancer that has recurred following surgery or radiation and is the standard of care for men with metastatic prostate cancer. ADT inhibits testosterone production or blocks activation of the androgen receptor, depending on the specific drug employed.
About 90% of men respond to ADT initially, but nearly all individuals with recurrent or metastatic cancer will eventually develop castration-resistant prostate cancer (CRPC). That’s largely because prostate cancer tumors continue to produce androgens even during active therapy.
Hormone therapy, part 2
For men with non-metastatic CRPC, the U.S. Food and Drug Administration has approved three antiandrogen drugs in the last two years to address resistance to first line ADT—apalutamide, darolutamide, and enzalutamide. All target the androgen receptors and block the stimulating effect of testosterone and other hormones on prostate cancer tumors. Clinical trials have demonstrated longer overall survival, extended time to increased pain, and increased time to metastatic disease development for these drugs.
The new therapies are not without significant side effects, however. Fatigue and joint pain are common in all three, while apalutamide also increases the risk of falls and fractures, seizure, heart disease, and stroke. Enzalutamide raises the risk of seizure, posterior reversible encephalopathy syndrome (PRES), as well as allergic reactions, falls and fractures, and heart disease. Side effects for darolutamide include decreased white blood cell count and changes in liver function tests.
Options for metastatic cancer
“When prostate cancer metastasizes to another location in the body, it is in most cases incurable and the goal of treatment is to improve a patient’s symptoms or function, or to extend the length of the patient’s life,” said the FDA’s Suzman.
Treatments available that provide a survival benefit for metastatic prostate cancer include docetaxel, which stood alone for more than a decade. In addition to the three antiandrogen drugs approved for non-metastatic CRPC as well as metastatic CRPC, a host of newer therapies including several immunotherapies and poly (ADP-ribose) polymerase (PARP) inhibitors have been added to the armamentarium more recently to treat advanced cancers.
Because of the overlap between drugs used for metastatic and non-metastatic CRPC, the National Comprehensive Cancer Network moved away from recommending first and subsequent lines of therapy. As of 2021, the guidelines instead recommend therapies based primarily on prior treatment exposure.
For patients who are docetaxel and novel hormone therapy naïve, the National Comprehensive Cancer Network (NCCN) Guidelines for Advanced-Stage Prostate Cancer (1.2021) recommends abiraterone, docetaxel and enzalutamide as preferred treatments, with sipuleucel-T, an immunotherapy, and radium-223 are also preferred options in specific circumstances.
For patients who have previously received docetaxel but not a novel hormone therapy, the preferred therapies are abiraterone, cabazitaxel and enzalutamide. Mitoxantrone is recommended for palliation in symptomatic patients who cannot tolerate other therapies, radium-223 for patients with bone metastases, and pembrolizumab in other circumstances.
When patients have received novel hormone therapy but not docetaxel, the guidelines prefer docetaxel and sipuleucel-T, with olaparib, cabazitaxel/carboplatin, pembrolizumab, radium-223, and rucaparib in specific situations. Other recommended therapies in this setting include abiraterone plus dexamethasone, enzalutamide, and other secondary hormone therapies.
Preferred regimens for individuals who have had both docetaxel and novel hormone therapy previously include cabazitaxel and docetaxel rechallenge. Certain patients could benefit from olaparib, cabazitaxel/carboplatin, pembrolizumab, mitoxantrone, radium-223, and rucaparib. Abiraterone, enzalutamide and other secondary hormone therapies are also recommended.
Emerging options
The large number of therapies under study indicate that the options for prostate cancer treatment will continue to grow. Both novel small molecules and radioligand therapies have recently shown promise.
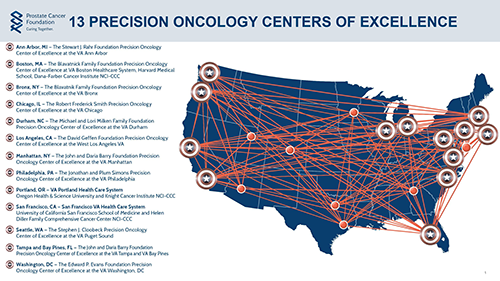
At the VA, connecting veterans to those studies is a priority. As part of that commitment, the Centers of Excellence have expanded the availability of genomic testing to help match patients to the most appropriate treatments and trials.
“VA has launched several efforts to level the playing field for veterans to access clinical trials for innovative prostate cancer therapies,” said Isla P. Garraway, MD, PhD, an attending urologist and translational researcher at the Greater Los Angeles VA Healthcare System. “This is a win-win for veterans and for research, allowing the diverse veteran population to participate in these trials and researchers to confirm that the findings from these studies are relevant across racial/ethnic groups.”
- Wilt TJ, Ullman KE, Linskens EJ, MacDonald R, Brasure M, Ester E, Nelson VA, Saha J, Sultan S, Dahm P. Therapies for Clinically Localized Prostate Cancer: A Comparative Effectiveness Review. J Urol. 2021 Apr;205(4):967-976. doi: 10.1097/JU.0000000000001578. Epub 2020 Dec 22. PMID: 33350857.

