 LA JOLLA, CA — When the Prostate Cancer Foundation entered into a partnership with the VA to fight the common condition, an added benefit was the stepped-up effort to increase the number of minority patients enrolled in PCF studies.
LA JOLLA, CA — When the Prostate Cancer Foundation entered into a partnership with the VA to fight the common condition, an added benefit was the stepped-up effort to increase the number of minority patients enrolled in PCF studies.
African Americans are 64% more likely to develop prostate cancer and more than twice as likely to die from the disease than other men overall, although they fare better in equal-opportunity healthcare systems such as the VA. Prostate cancer represents more than 40% of all diagnosed cancers in African American veterans compared to 26% of cancers in white veterans.1
“One of the unique things about the VA is the patient population,” Kenute Myrie, PhD, scientific program manager of oncology, VA Office of Research and Development, told U.S. Medicine recently. “We have one of the highest concentrations of African Americans in a large, integrated healthcare system. African Americans are disproportionately affected by prostate cancer, yet in most clinical trials the number of African Americans forms a very low percentage of participants. Increasing enrollment in trials at the VA will be very meaningful for the community, particularly as African Americans have a more heterogenous genetic background than whites in most trials.”1
In general, according to current, Black men who receive prostate cancer screening and care at the VA have much better outcomes than those using community care.
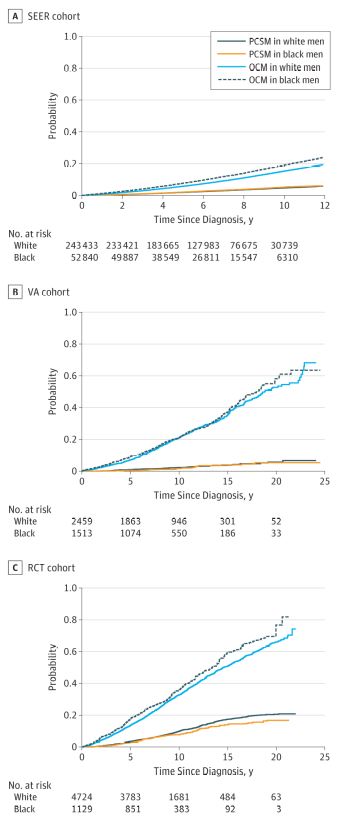
A study two years ago in JAMA Oncology determined, “In this multiple-cohort study of 306 100 patients with prostate cancer, black race was not associated with inferior prostate cancer-specific mortality in cohorts from Veterans Affairs health system and National Cancer Institute-sponsored randomized clinical trials. Black race was associated with increased prostate cancer-specific mortality within the Surveillance, Epidemiology, and End Results U.S. population registry, but not in the high-risk subgroup after baseline covariable adjustment, although black race remained associated with increased other-cause mortality.”1
The University of Michigan-led authors explained that similar access to care and standardized treatment erased inequities in death rates for Black patients at the VHA with nonmetastatic prostate cancer, stating that those veterans “appeared to have comparable stage-for-stage prostate cancer-specific mortality to white men.”
A more recent study conducted among veterans signaled a way forward to help erase the survival disparity for African American (AA) men compared to non-Hispanic white men.
The research available at the recent American Society of Clinical Oncology’s 2021 annual meeting pointed out that Black men are poorly represented in the prostate-specific antigen screening studies on which evidence-based prostate cancer screening guidelines are based. To find out how that affected the cohort in question, the study team examined associations of PSA screening intensity with disease severity at diagnosis and prostate cancer-specific mortality (PCSM) in African American men younger than 55.2
Noting that the earliest recommended age to begin discussion of PSA screening is 40, the authors identified AA men aged 40-55 years, diagnosed with prostate cancer from 2004 to 2017 within the VHA. The cohort included 4,654 men, mean age 51.8, with mean PSA screening rate of 53.2%. For the study, the median prediagnostic observation period was five years, and median follow-up was seven years.
At diagnosis, there was a higher prevalence of Gleason sum 8 or greater (Grade Group ≥ 4) and metastatic disease in the ”low” group compared with to the “high” group—Gleason sum 8 or greater (Grade Group ≥ 4)]: 18.6% vs. 14.4%, p < 0.01. Metastatic disease at diagnosis was 3.7% vs. 1.4% in the low vs. high group, respectively.
PSA Screening
Researchers pointed out that Increased PSA screening intensity was associated with significantly reduced odds of metastatic disease at diagnosis (odds ratio: 0.61, 95% confidence interval (CI) = [0.47-0.81], p < 0.01) and decreased risk of PCSM (sub-distribution hazard ratio: 0.75, 95% CI = [0.59-0.95], p = 0.02)
“In this large national cohort of AA men aged 40 to 55 years, PSA screening increased intensity was associated with decreased risk of lethal disease and metastases at time of diagnosis and decreased PCSM,” the authors wrote. “These data support the hypothesis that PSA screening and early prostate cancer detection may improve outcomes in younger AA men.”
But what happens when cancer is diagnosed? Another area of concern has been the growing use of conservative management and how that has differed somewhat among white and African American patients, even at equal-opportunity healthcare systems such as the VHA.
In general, clinical guidelines recommend conservative management, either active surveillance or watchful waiting, for men with low-risk and intermediate-risk prostate cancer. Use of conservative management can be controversial, however, for African American patients, who have worse prostate cancer outcomes compared with white patients.
A study published in JAMA Network Open last year evaluated the association of African American race with the receipt and duration of conservative management at the VA.
For the cohort study, Corporal Michael J. Crescenz VAMC-led researchers used data from the VA Corporate Data Warehouse for 51,543 African American and non-Hispanic white veterans diagnosed with low-risk and intermediate-risk localized node-negative prostate cancer between Jan. 1, 2004, and Dec. 31, 2013, with analysis from Feb. 1 to June 30, 2020.3
All patients received either definitive therapy—prostatectomy, radiation, androgen deprivation therapy—or conservative management—active surveillance or watchful waiting—according to the study. The focus was on patients who received conservative management and, for that group, time from diagnosis to definitive therapy. Participants were a median age of 65 (61-70) years, and 28.8% were African American veterans.
Results indicated that, compared with white veterans, African American veterans were more likely to have intermediate-risk disease (18 988 [51.7%] vs. 8526 [57.5%]), three or more comorbidities (15 438 [42.1%] vs. 7614 [51.3%]) and high disability-related or income-related needs (9078 [24.7%] vs 4614 [31.1%]).
Researchers pointed out that, overall, 20,606 veterans (40.0%) received conservative management. Yet, they added, African American veterans with low-risk disease (adjusted relative risk, 0.95; 95% CI, 0.92-0.98; P < 0.001) and intermediate-risk disease (adjusted relative risk, 0.92; 95% CI, 0.87-0.97; P = 0.002) were less likely to receive conservative management than white veterans.
Specifically, compared with white veterans, African American veterans with low-risk disease (adjusted hazard ratio, 1.71; 95% CI, 1.50-1.95; P < 0.001) and intermediate-risk disease (adjusted hazard ratio, 1.46; 95% CI, 1.27-1.69; P < 0.001) who received conservative management were more likely to receive definitive therapy within five years of diagnosis (restricted mean survival time [SE] at five years, 1679 [5.3] days vs. 1740 [2.4] days; P < 0.001).
“In this study, conservative management was less commonly used and less durable for African American veterans than for white veterans,” the authors concluded. “Prospective trials should assess the comparative effectiveness of conservative management in African American men with prostate cancer.”
- Dess RT, Hartman HE, Mahal BA, et al. Association of Black Race With Prostate Cancer-Specific and Other-Cause Mortality. JAMA Oncol. 2019;5(7):975–983. doi:10.1001/jamaoncol.2019.0826
- Qiao E, Kotha NV, Nalawade V, Qian A, et. Al. (June 4-8) Association of increased intensity of prostate-specific antigen screening in younger African American men with improved prostate cancer outcomes. ASCO 2021. Virtual
- Parikh RB, Robinson KW, Chhatre S, Medvedeva E, Comparison by Race of Conservative Management for Low-Risk and Intermediate-Risk Prostate Cancers in Veterans From 2004 to 2018. JAMA Netw Open. 2020 Sep 1;3(9):e2018318. doi: 10.1001/jamanetworkopen.2020.18318. PMID: 32986109; PMCID: PMC7522702.
