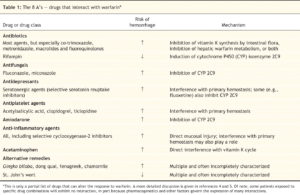
Drug Interactions for Warfarin
Source: CMAJ August 14, 2007 177 (4) 369-371; DOI: https://doi.org/10.1503/cmaj.0709
IOWA CITY, IA — About one-third of VA patients have three or more chronic conditions.1 Ironically, for many of them, that complexity makes choosing between warfarin and a direct acting oral anticoagulant easier.
“The presence of multiple chronic conditions often means that patients are on several prescription medications,” said Mary S. Vaughn Sarrazin, PhD, investigator, Center for Access and Delivery Research and Evaluation based at the Iowa City VAMC, and associate professor of internal medicine at the Roy and Lucille J. Carver College of Medicine at the University of Iowa. “DOACs are believed to have fewer interactions with other drugs than warfarin, which may make them safer for patients with very complex medication regimens.”
Some conditions may make the decision to use any anticoagulant more fraught, however. “Some patients may have conditions that impact both bleeding and stroke risk. In those patients, it may be difficult to determine whether the benefits of improved stroke prevention outweigh the increased risk of dangerous hemorrhage associated with anticoagulants,” she told U.S. Medicine.
While the U.S. Food and Drug Administration provides guidance for anticoagulant choice in the presence of renal disease, guidelines are “not explicit with respect to anticoagulation therapy in patients with more complex illness,” she said.
To help clinicians determine the best choice for patients with multiple comorbidities, Sarrazin and her colleagues at the Carver College of Medicine evaluated the outcomes of treatment with warfarin and the DOACs dabigatran and rivaroxaban in nearly 22,000 Medicare patients diagnosed with atrial fibrillation between 2010 and 2013.2
The team found no difference in stroke rates between the three medications.
Dabigatran had a 38% lower risk of major hemorrhage compared to warfarin in patients with a low Gagne comorbidity score and similar risk of major bleeding in patients with moderate to high comorbidity scores. Rivaroxaban had similar rates of major hemorrhage compared to warfarin in all groups but higher risk compared to dabigatran in patients with medium and high morbidity scores.
Both rivaroxaban and dabigatran users had significantly lower mortality risk than warfarin users.
Because the DOACs apixaban and edoxaban came on the market after the start of the study, the researchers did not include them in the analysis, but they are likely to have similar results. “Clinical trials for apixaban and edoxaban both found a mortality advantage over warfarin,” Sarrazin said. “While results from clinical trials do not always translate to clinical practice, we have no reason to believe that the same mortality advantage would not exist in clinical practice.”
Several clinical trials have demonstrated a lower risk of bleeding for apixaban than other DOACs and warfarin “Edoxaban, dabigatran and rivaroxaban have been shown to have higher risk of gastrointestinal bleeding compared to warfarin. Current VA guidelines suggest that physicians consider apixaban over other DOACs in patients with a history of bleeding or factors associated with increased risk of bleeding,” she added.
Still, warfarin may be the best option for some patients. “There’s an increasing trend of DOAC use in VA,” Sarrazin noted. “However, warfarin is still recommended for patients with severe renal impairment or patients with mechanical heart valves. Moreover, DOACs may have intolerable side effects such as dyspepsia—making warfarin a more tolerable option. Finally, physicians and patients may prefer the monthly monitoring required with warfarin use to assess anticoagulant activity in complex patients where relative risks and benefits of anticoagulation are particularly unclear.”
- Yoon J, Zulman D, Scott JY, Maciejewski ML. Costs associated with multimorbidity among VA patients. Med Care. 2014 Mar; 52 Suppl 3:S31-36.
- Mentias A, Shantha G, Chaudhury P, Sarrazin MS. Assessment of Outcomes of Treatment with Oral anticoagulants in patients with Atrial Fibrillation and Multiple Chronic Conditions: A Comparative Effectiveness Analysis. JAMA Netw Open. 2018 Sept 7; 1(5):e182870.
