Fivefold Increase in Two Decades
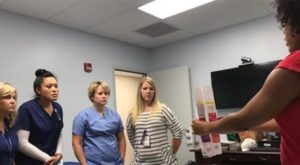
VA’s Women’s Health Services (WHS) provides a Women’s Health Mini-Residency for Primary Care Rural Providers and Nurses. In this photo, a nurse instructor shows VA nurses at the Murfreesboro, Tenn., VA Medical Center contraceptive options available to women veterans. Photo from May 26, 2020, VAntage Point blog.
WASHINGTON — The Deborah Sampson Act represented a major advance for women’s health care at the VA, an area long neglected despite the steady rise in the number of women serving in the U.S. military over the last several decades.
Speaker of the House Rep. Nancy Pelosi (D-CA) characterized the act as “the most comprehensive women veterans’ bill in over a decade,” based on its depth and breadth. The act mandated creation of a dedicated Office of Women’s Health at the VA to monitor health initiatives across the complex organization and develop standards of care specific to the issues women veterans face.
Today, women represent 15% of active duty military members, 18% of the Guard and Reserves and 10% of veterans. The number of women veterans receiving care from the VA has increased five-fold, rising from 159,000 in 2000 to 756,000 in 2019. Women veterans have an average age of 51 compared to an average age of 65 for men.
Close to 45% of women veterans who receive care through VHA were aged 18 to 44 years old and likely to require a range of health services specific to women of childbearing age. “The majority of women veterans require family planning resources, prenatal and maternity care, or premenopause and perimenopause care,” said Tammy Bartlet, associate director, National Legislative Service, Veterans of Foreign Wars of the United States at a congressional hearing on implementing the Deborah Sampson Act.
The act took called for concrete steps to improve the provision and access of health services for women. Among other requirements, each VAMC and clinic must have at least one primary care provider focused specifically on women’s health. Each facility is also now mandated to hold regular public forums to solicit feedback from women veterans and to conduct focus groups to ensure the center’s services are addressing the needs of women veterans.
Increasing training in women’s health and certifying providers who have completed it increases women veterans’ trust and comfort in the care provided. “Thirty-eight percent of women veterans who have access to and use a Veterans Health Administration (VHA) women veteran’s health clinic were very satisfied” with their care, Bartlet noted. “Only 14% of women veterans who do not have access to a woman veteran’s health clinic were very satisfied with their care.”
Training in Women’s Health
Even as VAMCs and clinics ramp up to deliver gender-specific care and retrofit facilities, the VA has significantly expanded its training programs for primary care providers and nursing staff. A “mini-residency” offered by the Women’s Health Services combines online courses on topics such as abnormal uterine bleeding, contraception, breast issues, pelvic pain, screening for breast and cervical cancer and intimate partner violence. Other topics covered include the physical demands and injuries associated with heavy gear, military sexual trauma, combat exposure, deployment challenges and post-deployment adjustments specific to women.
The on-site component takes an interactive approach, with case discussions, medical mannequins for hands-on simulations, videos of procedures and exams, and gynecologic teaching associates for the breast and pelvic exams as well as the training on taking a thorough patient history that includes women’s health concerns.
The Office of Rural Health delivers the in-person segment on-site at rural clinics in recognition of the challenges faced by facilities with small staffs, where off-site education creates a serious disruption in services. Members of rural care teams can complete the online components independently ahead of in-person training and then participate in a one-day training at their clinic. Taking the program on the road allows the VA to meet the needs of the 26% of women veterans who live in rural areas. The VA has also continued to expand its telehealth services to provide care to these women and other veterans.
Providers and nurses train together to practice the interactions appropriate to this setting, and each participant receives 18 hours of training credit. Physicians who complete the training are designated Women’s health primary care providers (WH-PCPs).
Continued expansion of the training program will help the VA address one of the most common requests of women veterans. “The overwhelming majority of women veterans want VA to expand access to women-specific health care, which includes hiring more VA health care professionals who are able to identify and treat their unique health care needs,” according to the Veterans of Foreign Wars. “More specifically, women veterans want the opportunity to receive their health care from women health care providers.”
One of the other hot topics for women is contraception. “Women veterans who use VA health care for family planning services are also concerned that VA requires co-payments for preventative prescription drugs, such as contraceptives,” the VFW noted. “This is counter to industry standards for private health insurance plans, which do not require out-of-pocket costs for preventative care prescriptions.”
Under the Affordable Care Act, basic contraceptives are provided to women with civilian health insurance with no co-pay. Tricare also offers access to contraception without co-pays. The Equal Access to Contraception for Veterans Act passed the House in June and has been referred to the Senate’s Committee on Veterans Affairs.
