By Annette M. Boyle
 WASHINGTON—Concerned about how much time clinicians spend reading and responding to emails, the VA is changing its messaging system so that more of their focus can be on patient care.
WASHINGTON—Concerned about how much time clinicians spend reading and responding to emails, the VA is changing its messaging system so that more of their focus can be on patient care.
The new approach to the inbox notifications system, developed in response to concerns expressed by providers, was announced late last year.
“The number of computerized notifications currently delivered to clinicians is excessive compared to industry standard and is a major complaint from providers,” explained Sheila A. Ochylski, DNP, RN, chief nursing informatics officer for the VA and the executive sponsor of the effort.
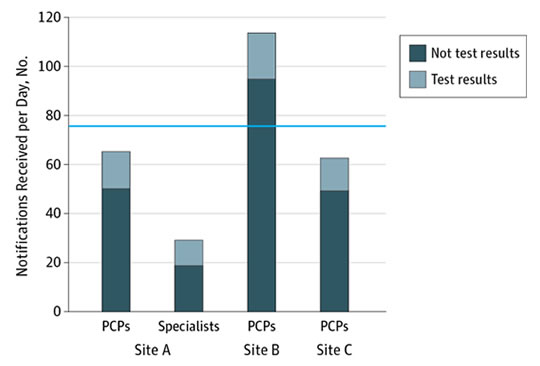
Quantities and Types of Notifications Received by Site and Physician RolePrimary care providers (PCPs) received an overall mean of 76.9 notifications per day (blue line). Specialists (site A only) received a mean of 29.1 notifications per day (P < .001).
While the messaging system initially was designed to share clinical information, such as test results or referrals, facilitate communication between providers and transmit refill requests, other kinds of less-useful messages have made finding crucial emails more difficult and time-consuming.
“The public never sees the excessive amount of emails and alerts that take up a doctor’s time,” pointed out VA Secretary David J. Shulkin, MD. “Some of it is necessary, but other emails do nothing to advance patient care and can, in fact, pose a major safety hazard because of lesser important emails. We want our doctors to have the right information they need to provide quality health care to veterans, and this is a step in the right direction.”
A survey of 2,590 primary care providers in the VA found that nearly 70% said they received “more alerts than they could effectively manage,” and almost 30% reported that they had “personally missed results that led to care delays.”1
Researchers at the Michael E. DeBakey Veterans VAMC in Houston calculated that clinicians take about 52 seconds to process each electronic health record (EHR) notification, according to a research letter published in JAMA Internal Medicine in 2016. Using that figure, the research team estimated that those notifications alone consume more than an hour a day for primary care providers. Specialists receive less than half the number of messages, they noted.2
For primary care providers, the high number of notifications makes “it harder to discern important vs. irrelevant information and [increases] their risk of overlooking abnormal test results,” the Houston team noted in their study. To ensure that important messages receive appropriate attention, the researchers recommended adopting “strategies to help filter messages relevant to high-quality care, EHR designs that support team-based care, and staffing models that assist physician in managing this influx of information.”
The VA project appears to be taking that suggestion to heart. The changes to the messaging system implemented so far, plus an educational component that trains clinicians to optimize their inbox, have reduced the time clinicians spend on these communications by an hour and a half a week, according to the VA.
Paperwork vs. Patient Care
That gives providers more time to spend with patients and properly consider their care, which has been a challenge for providers at the VA and elsewhere. “Time spent by clinicians to follow up on important veteran care information that may require prompt attention is our primary concern,” Ochylski told U.S. Medicine. Clearing out the inbox shifts time from paperwork to patient care.
Nationwide, physicians spend about two hours on administrative work for every hour they spend on patient care, according to a study published in the Annals of Internal Medicine. 3 The nonpatient care hours detract from the most rewarding aspects of providers’ work and increases fatigue and burnout, the VA said.
While House Fellow Tina Shah, MD, led the streamlining project along with a small task force of experienced providers. This team identified best processes and practices for the use of notifications and messages, monitored the number of computerized messages and determined the best ways to deliver them, Ochylski said.

VA care team members Dr. Faraz Afridi, MD, Niharika Chimalakonda, MD, and Israel Acosta Sanchez, MD, review their VA-issued tablet devices, which they use to help intake patients to the Orlando, FL VAMC. VA photo.
To improve the process further, the task force has joined forces with electronic health record specialists to identify ways to electronically screen out nonurgent items, she added.
“The long-term goal of the current project is to apply clinical decision support methods to develop and implement processes to decrease clinician documentation burden and increase time spent with direct patient care,” Ochylski said. “Additionally, we have identified a number of specific opportunities for innovation in the presentation of electronic health messaging and are now establishing a process where improvements can be sustained and monitored.”
While improvements should make the system even better, the project has already been a home run in terms of clinician satisfaction. “The response from clinicians has been overwhelmingly positive,” Ochylski said.
The acceptance reflects the project’s alignment with providers’ needs and goals. “This is an opportunity to combine approaches that provide clinicians fast and easy access to the data they most frequently seek. Simultaneously, they can capitalize on the opportunity to provide relevant clinical reminders with limited disruption to clinician workflow,” she added.
“When we let doctors do what they do best—giving care to Veterans—we know it improves the care they receive,” Secretary Shulkin added. “It’s why VA is one of the best places to work and why our doctors have lower burnout rates than the private sector. This initiative is just one of many underway for VA to address clinician burnout and improve the quality of our care.”
- Singh H, Spitzmueller C, Petersen NJ, Sawhney MK, Sittig DF. Information overload and missed test results in electronic health record-based settings. JAMA Intern Med. 2013 Apr 22;173(8):702-4.
- Murphy DR, Meyer AN, Russo E, Sittig DF, Wei L, Singh H. The burden of inbox notifications in commercial electronic health records. JAMA Intern Med. 2016;176(4):559-560.
- Sinsky C, Colligan L, Li Ling, Prgomet M. Reynolds S, Goeders L, Westbrook J, Tutty M, Blike G. Allocation of physician time in ambulatory practice: A time and motion study in four specialties. Ann Intern Med. 2016;165(11):753-760.

Thank you so much for looking at this problem. Coming from a private sector, the amount of time required for alerts is overwhelming. Those processed in 52 seconds must not include med changes, medication reconciliation sheets, and notification of the veteran, as many of mine do. I see no reason why the nurse can’t relay some of this information, as directly outlined (documented) by the provider and then if questions, refer to the provider.
As a CBOC working under the auspices of an enterprise, we get emails about things happening in the main facility that has no impact on the CBOCs.
This is the best news I’ve heard in the 2.5 years I’ve been with the VA!
Duplicate alerts should be collated so duplicate work is not caused by alerts. This is a big problem when numerous alerts are placed in sequence in a short time. There can be 3,4 or more alerts about the same issue and same problem on same patient with each alert needing to be addressed or deleted.
We need a software fix that would eliminate useless alerts regarding consults that we order like, “first attempt to schedule”, “second attempt to schedule”, etc. I must sift through all these alerts to avoid missing the rare alert requiring me to order a “nonVA funding” consult or perform a necessary intervention to prevent the consult thread from breaking, causing the delay or loss of timely specialty care for my vet. Please let me know when this has been accomplished. I’ll beta test it!
Sign me up now!
An inordinate amount of clinician time is spent on required annual and Biannual training. It will be useful to quantitate time spent by all clinicians on training instead of patient care, and adjust training accordingly
As a VA PC provider I was waiting for those above mentioned changes for long time. Specially huge number of alerts interfere with pt care.
Thanks for focusing at this matter.
As a VA PC provider I was waiting for those above mentioned changes for long time. Specially huge number of alerts interfere with pt care.
Thanks for focusing at this matter.
We need a software fix that would eliminate useless alerts regarding consults that we order like, “first attempt to schedule”, “second attempt to schedule”, etc. I must sift through all these alerts to avoid missing the rare alert requiring me to order a “nonVA funding” consult or perform a necessary intervention to prevent the consult thread from breaking, causing the delay or loss of timely specialty care for my vet. Please let me know when this has been accomplished. I’ll beta test it!
Sign me up now!
Duplicate alerts should be collated so duplicate work is not caused by alerts. This is a big problem when numerous alerts are placed in sequence in a short time. There can be 3,4 or more alerts about the same issue and same problem on same patient with each alert needing to be addressed or deleted.
An inordinate amount of clinician time is spent on required annual and Biannual training. It will be useful to quantitate time spent by all clinicians on training instead of patient care, and adjust training accordingly
Thank you so much for looking at this problem. Coming from a private sector, the amount of time required for alerts is overwhelming. Those processed in 52 seconds must not include med changes, medication reconciliation sheets, and notification of the veteran, as many of mine do. I see no reason why the nurse can’t relay some of this information, as directly outlined (documented) by the provider and then if questions, refer to the provider.
As a CBOC working under the auspices of an enterprise, we get emails about things happening in the main facility that has no impact on the CBOCs.
This is the best news I’ve heard in the 2.5 years I’ve been with the VA!