By Sandra Basu
WASHINGTON—VA officials sought to reassure lawmakers that the agency is responding appropriately to an oversight report finding that several medical providers who gave harmful care to patients were never reported to the National Practitioner Data Bank (NPDB) or state licensing boards (SLB).
One step, according to Gerard Cox, MD, MPH, VA acting deputy under secretary for health for organizational excellence, is that the range of clinical occupations that VA will report to the NPDB will be voluntary expanded.
“We are doing this because we feel this is the right thing to do for veterans,” Cox said.
While the NPDB only requires reporting physicians and dentists for adverse privileging actions and resignation while under investigation, VA plans to report “all privileged providers to the NPDB for privileging actions resulting from substandard care, professional misconduct or professional incompetence,” he testified at a House subcommittee hearing titled, “Examining VA’s failure to address provider quality and safety concerns.”
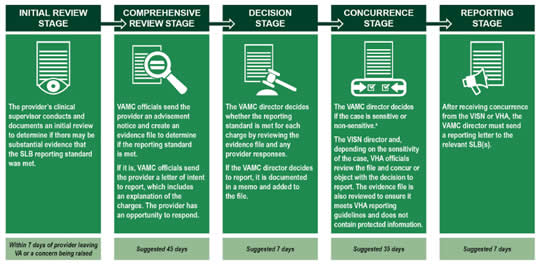
[Click to Enlarge]
An Overview of the Stages of the Veterans Health Administration’s (VHA) State Licensing Board Reporting Process
A case is considered sensitive if (a) it includes a previous history of licensure action against the provider; (b) it includes the death of a patient; (c) the provider has retained legal counsel in anticipation of litigation; (d) there has been media attent ion related to some aspect of the case; or (e) the provider has a clinical diagnosis, or is under the care of a physician, and that information is part of the review or provider response includes the provider’s personal health information.
Government Accountability Office (GAO) officials talked about the bigger issue. “VA’s failure to report the providers to the databank or state licensing boards makes it possible for providers to obtain privileges at other VAMC or non-VA healthcare entities that serve veterans,” explained Randall Williamson, the oversight group’s director of healthcare.
Specifically, the GAO looked at five VAMCs, finding that clinical care by 148 providers required reviews after concerns were raised about quality, but no documentation was available for about half of those reviews to prove they had been conducted.
Even many reviews that had been performed were not done so in a timely manner, the report added. Of the 148 providers, the VAMCs did not initiate reviews of 16 providers for three months, and in some cases, “for multiple years, after concerns had been raised about the providers’ care.”
Poor Oversight
Williamson told lawmakers that these situations were allowed to occur “largely because of poor oversight and accountability from top to bottom in the VHA hierarchy.”
“For example, neither the VISN nor the VA central office officials routinely perform any oversight to ensure that reviews are conducted in a timely way,” he pointed out.
From October 2013 through March 2017, the five VAMCs reviewed had only reported one of nine providers required to be reported to the NPDB according to VHA policy, the GAO report noted.
“The VA medical centers documented that these nine providers had significant clinical deficiencies that sometimes resulted in adverse outcomes for veterans,” report authors wrote “For example, the documentation shows that one provider’s surgical incompetence resulted in numerous repeat surgeries for veterans.”
Providers were not reported to the NPDB and state licensing boards as required, the GAO concluded, because “VA medical center officials were generally not familiar with or misinterpreted VHA policies related to NPDB and state licensing board reporting” and that “VHA policy does not require the networks to oversee whether VA medical centers are reporting providers to the NPDB or state licensing boards when warranted.”
Cox told lawmakers that he “shares” their concerns regarding the issues and that the agency is updating and rewriting policies in response to the GAO’s report. “We need to do much better. I can’t excuse the fact that in the past that adequate oversight by VISNs and the central office has not been provided,” he said.
One problem, he added, is the “lack of clarity about the roles and responsibilities” of the VISNs in handling the reporting of medical providers, suggesting, “We have to do a better job of communicating these requirement and educating those we put into leadership positions.”
Among the steps VA plans to take are improving the timeliness of reviews and reporting, and improving the agency’s oversight to ensure that no settlement agreement waives VA’s ability to report providers to NPDB or SLBs, he said in a written statement, explaining, “Any VA employee who enters into a settlement agreement waiving VA’s ability to report to NPDB or SLBs will be subject to discipline.”
Lawmakers showed little restraint in criticizing the agency.
“The fact that VA is taking three months to, and in some cases years to, review quality concerns, is entirely unacceptable. But perhaps more outrageous is the cases where VA uses taxpayer dollars to settle cases with clinicians who have provided substandard care to essentially just make them go away,” said Chairman Rep. Jack Bergman (R-MI) of the House Committee on Veterans Affairs Oversight and Investigations Subcommittee.
Rep. Bruce Poliquin (R-ME) described a past case where VA did not report a dangerous provider in a timely fashion, leading to multiple patients suffering harm. “You all are not reporting on time to make sure that no one else gets hurt. I think you all are protecting your butts,” he said.
In addition, House Committee on Veterans’ Affairs Chairman Rep. Phil Roe (R-TN) said it “shocked him” that 148 providers needed to be reviewed in the five medical centers, with only one reported to the NPDB.
“We don’t know how pervasive it is because we just did a small sample of the physicians in the VA system, just five medical centers,” he said.
He and his colleagues have introduced a bill that “directs the Department of Veterans Affairs (VA) to ensure that each VA physician is informed of the duty to report any covered activity committed by another physician that the physician witnesses or otherwise directly discovers to the applicable state licensing authority within five days.”
