Click To Enlarge: Rates of emergency department (ED) visits and/or hospital admission within 1 year by opioid series …
WASHINGTON — From 2012 to 2020, VA reduced prescription opioid use in patients in its healthcare system by 64% — from 679,000 veterans to 247,000. During that time, patients receiving opioids and benzodiazepines together have decreased 87%, and the number of patients on long-term opioid therapy has plunged 70%.
This reduction is an effort to stem the tide of opioid addiction that disproportionately affects veterans and servicemembers. Previous studies have found veterans are twice as likely to die of an opioid overdose compared to the general population, and, while active duty servicemembers are less likely to use illegal drugs, they are more likely to abuse prescription drugs.
VA’s success in reducing opioid prescribing has been due to a combination of increased patient and provider education, as well as an increase in alternative pain relievers. Studies show that a similar combination of education and medication could be effective for patients already suffering from opioid use disorder (OUD).
A recent study conducted by the VA St. Louis Healthcare System found medication-assisted therapy (MAT) works better when it goes hand in hand with patient education and that education alone resulted in significant decreases in patients showing up in the emergency room and admitted to the hospital.
According to the researchers, whose study was published recently in the American Journal of Health System Pharmacy, though guidelines recommend that all patients with OUD be offered MAT, only about 20% of patients have received any specialty addiction treatment. Less than half of privately funded substance abuse disorder treatment programs offer MAT and, of those, only 33% of patients with OUD receive MAT. Little was in the literature about the factors influencing patients’ decision to try MAT.1
In 2016, the St. Louis VA began offering a new series of patient education groups specific to OUD as part of its inpatient substance abuse rehabilitation program. The program—referred to in the study as “the opioid series”—consisted of four one-hour group sessions that focused specifically on OUD. They incorporated motivational interviews, cognitive behavioral therapy and medication education to help patients make informed decisions. Three of the sessions were led by psychologists and social workers, while the fourth was led by a clinical pharmacist. The pharmacist provided education on MAT and the role of naloxone rescue kits for overdose.
The researchers analyzed a group of OUD patients who had been in the rehabilitation program between 2014 and 2018 and compared those who had taken part in the opioid series with those who had not.
The analysis found that patients who received the intervention began MAT at a rate of 74.6% compared to 25.3% in the control group. Naltrexone long-acting injection products were prescribed to 53% of the intervention group compared to 20.8% in the control, and receipt of a naloxone rescue kit prescription was twice as likely in the intervention group (85.7% compared to 42.1%).
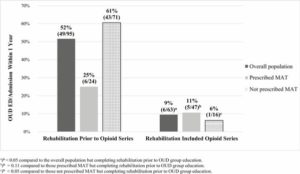
Those who took part in the four education sessions were also significantly less likely to show up in the hospital in the following year for reasons associated with their OUD (9.5% compared to 51.6%). However, that lower rate seems to be connected more to the increase in patient education and occurs regardless of whether the patient initiates MAT.
While MAT utilization was associated with a lower rate of hospitalization in the population overall, the analysis showed that in the intervention group this wasn’t true. The rate of admission for patients in the intervention group utilizing MAT was 10.6% compared to 6.3% for those who did not choose to use MAT.
The greatest difference comes when comparing hospital admission for patients not utilizing MAT was between the control and intervention groups—60.6% compared to 6.3%. This suggests that education alone can help prevent hospitalization.
“In the intervention group, both those with and without MAT had a low rate of OUD ED/admission, and those without MAT had the lowest,” the researchers noted in their analysis. “Interestingly, multivariate regression estimated that participation in the opioid series had a larger association with decreased OUD ED/admissions than receiving MAT within the studied population.”
“Psychosocial interventions are recommended to be used in combination with MAT to improve outcomes,” the researchers added, “but less is known about which interventions may be of benefit in those who choose not to initiate MAT. The results of our study suggest that the interventions used in the opioid series may help to both increase rates of MAT and also to potentially provide independent improvement in outcomes.”
The study also found that another strength of the opioid series program is that it was implemented with existing providers.
“Providers who led the opioid series group sessions were already involved in the inpatient rehabilitation program,” researchers stated. “Utilization of existing staff makes implementation of this series potentially more feasible for other treatment program and facilities.”
- Kirby T, Connell R, Linneman T. Assessment of the impact of an opioid-specific education series on rates of medication-assisted treatment for opioid use disorder in veterans. Am J Health Syst Pharm. 2021 Feb 8;78(4):301-309. doi: 10.1093/ajhp/zxaa386. PMID: 33289022.

