LOS ANGELES — An expert panel has identified quality measures for ambulatory primary care for VHA patients who have complex care needs and are at high risk for adverse outcomes, such as hospitalization or death, according to a new study.
Despite efforts to improve healthcare quality for patients with complex needs who are at highest risk for hospitalization or death, no guidance seems to exist on what equals measurable high-quality care. It’s important to identify quality measures that are relevant to multiple chronic conditions and disease states to help healthcare professionals and healthcare systems better design and report on quality improvement efforts for these patients.
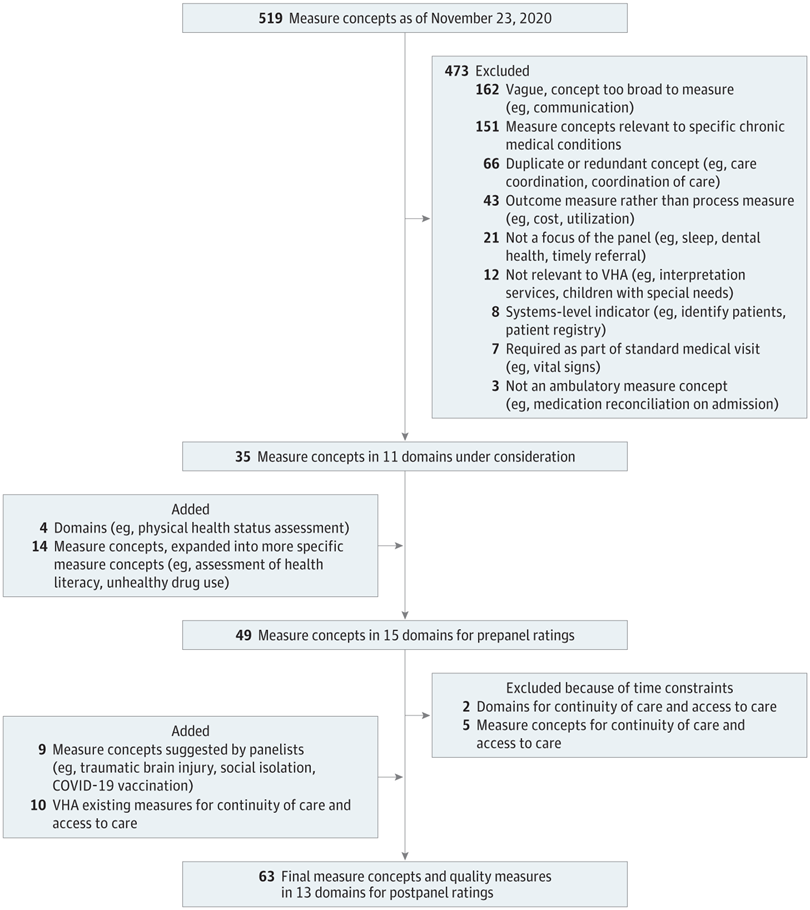
In the JAMA Network Open study, the authors performed a systematic review from June 2020 to June 2021 of published studies that suggested, evaluated or used indicators of quality care for patients at high risk of adverse outcomes. Concepts associated with single conditions, surgical or other specialty care settings, as well as inpatient care were excluded. The systematic review identified 519 measure concepts, and the list was shortened for the expert panel evaluation.1
A panel of 14 experts (10 VHA leaders and staff, two non-VHA physician investigators and two veterans) discussed and rated the importance of the remaining potentially relevant measure concepts using a modified RAND/UCLA Appropriateness Method from January to April 2021.
The panel first privately voted on clinical activities relevant for high-risk veteran care, then met to discuss their ratings and voted again on high-priority activities. Measure concepts were rated on a scale of one to nine, with nine being the highest priority. A median rating of 7.5 or greater was used as the cutoff to identify the highest-priority items.
“A small group of VA healthcare leaders, veterans and non-VA researchers were able to agree on some clinical activities that are important to improve outcomes for high-risk veterans,” according to study author Evelyn Chang, MD, MSHS, a physician and investigator at the VA Greater Los Angeles Healthcare System and associate clinical professor in the Geffen School of Medicine at the University of California at Los Angeles.
The panel’s recommendations to improve care for high-risk patients included timely assessment of housing instability, caregiver availability and support, physical function, depression symptoms and cognitive impairment; annual review of prescription regimens; primary care follow-up after emergency department visits and hospitalization; timely transmission of discharge information to primary care; and preventive care, including vaccinations for COVID-19 and pneumonia.
The study defined high-risk patients as those in the top 5 to 10 percent of risk for hospitalization and/or death. High-risk patients include those with multiple chronic conditions, mental health or substance use conditions, terminal diagnoses and unstable housing, as well as frail elderly individuals, Chang explained.
Quality measures are needed, because “healthcare providers and leaders have not agreed on the clinical activities that would be considered “high-quality care” for high-risk veterans,” Chang explained in an email to U.S. Medicine.
Care Improvement
“Identifying these clinical activities can translate to quality measures that may enable healthcare leaders to better design and evaluate programs to improve care for these patients,” Chang wrote.
The measured concepts with the highest median ratings focused on:
- Caregiver availability and support, COVID-19 vaccination and pneumonia vaccination (all rated 9.0);
- Housing instability (rated 8.5); and
- Physical function, depression symptoms, cognitive impairment, prescription regimen, primary care follow-up after an emergency department visit or hospitalization and timely transmission of discharge information to primary care (all rated 8.0).
The panel included 10 VHA staff members (physicians, nurse practitioners, a licensed clinical social worker, a registered nurse, and national program leaders in primary care, mental health and geriatrics), two non-VHA physician investigators (a physician investigator in the United Kingdom with expertise in quality measurement and a physician investigator from Kaiser Permanente with expertise in care for patients with complex healthcare needs) and two veterans who were receiving care at a VHA facility.
One of the patient panelists had participated in a prior VHA expert panel about patients with complex care needs. A second patient panelist had participated in other VHA expert panels related to primary care and was briefed on the purpose of this panel.
The panelists noted their greatest challenges were considering which measure concepts were feasible for primary care, actionable and relevant for the most high-risk patients.
Based on their knowledge, this is the first study that used a modified Delphi process to prioritize proposed measure concepts from a systematic review. Other studies have proposed quality measures for patients with complex needs, but existing performance measures were prioritized based on a model developed by experts.
This study has several limitations. The results are applicable only to the VHA setting and shouldn’t be generalized beyond, since the study was intended to improve care of high-risk veterans in the VHA. The panel also focused only on process measures and didn’t include outcome measures relevant to high-risk patients, which is typical when performance measurement is extended into a new area. In addition, the results are sensitive to the panel’s composition, and the proposed process measures are not intended to serve as accountability measures.
“Hopefully we can translate these high-rated clinical activities into quality measures that can inform future quality improvement efforts for complex, high-risk veterans,” Chang wrote.
Next, the study team will use the quality measures prioritized by the panel to develop potential electronic reminders or measures that build on existing VHA reports of primary care patients at high risk for hospitalizations or death. Reporting on these quality measures could enhance intensive management program evaluations and provide a set of targeted measures that healthcare systems can use to begin improving outcomes for high-risk patients, according to the study.
- Chang ET, Newberry S, Rubenstein LV, Motala A, Booth MJ, Shekelle PG. Quality Measures for Patients at Risk of Adverse Outcomes in the Veterans Health Administration: Expert Panel Recommendations. JAMA Netw Open. 2022 Aug 1;5(8):e2224938. doi: 10.1001/jamanetworkopen.2022.24938. PMID: 35917129.