ANN ARBOR, MI — Veterans who received intravenous ketamine treatments had improved symptoms of depression within the first 6 weeks, and these improvements were sustaine
d over at least 6 months with decreasing infusion frequency, according to a recent study.
The study published in The Journal of Clinical Psychiatry described “clinical outcomes of repeated infusions of intravenous ketamine in routine clinical practice and the frequency and number of infusions used to sustain symptom improvement of major depressive disorder.”1
Major depressive disorder is a “leading cause of disability worldwide, affecting an estimated 10% of the U.S. population annually,” according to the report. In VHA patients, “17% have a diagnosis of major depressive disorder, which is associated with increased morbidity from general medical conditions, such as diabetes and myocardial infarction, an increase in all-cause premature mortality and increased suicide mortality,” the researchers pointed out.
Even with antidepressant medications, “the majority of depression in VA patients has been observed to be chronic (e.g., duration of greater than two years), with remission relatively difficult to achieve,” according to the authors. A large clinical trial found that “VA patients who started a new antidepressant medication after at least one prior treatment attempt had remission rates of 16% across six months,” they explained. Oral “antidepressant medications also take several weeks to achieve response, resulting in a 50% reduction in symptoms,” study authors suggested.
Study authors were affiliated with the VA Ann Arbor, MI, Healthcare; the Albuquerque NM, VAMC; the VA Boston Healthcare System; Edward Hines Jr. VA Hospital in Hines, IL; VA San Diego Healthcare; VA Connecticut Healthcare System in West Haven, CT; and VA Office of Mental Health and Suicide Prevention in Washington, DC.
“Ketamine has gotten a lot of attention as a potential treatment for depression, but few studies have revealed how well it works in ‘real world’ settings, especially among the veteran population, where the majority of depression cases have been observed to be chronic, with remission relatively difficult to achieve,” according to lead author Paul Pfeiffer, MD, a research scientist and psychiatrist at the VA Center for Clinical Management Research and LTC Charles S. Kettles VAMC at VA Ann Arbor Healthcare System.
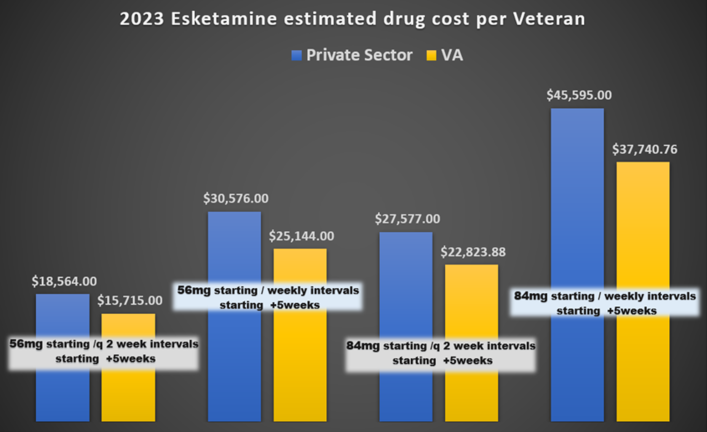
“There is also little long-term ketamine trial data,” Pfeiffer told U.S. Medicine. “However, use of ketamine, either intravenous ketamine or intranasal esketamine, has been growing steadily over the last five years. VA currently has 39 facilities offering treatments, up from 19 in 2020. In fiscal year 2023, more than 1,800 veterans received either IV ketamine or intranasal esketamine.”
In this study, the authors identified 215 veteran patients who received intravenous ketamine for depression in the VA system in fiscal year 2020. The patients were identified using VA’s national electronic medical record database and, according to the article, “98% had a past-year diagnosis of major depressive disorder, 12% had at least one major depressive disorder diagnosis with a psychotic features specifier and 2% had some other depressive disorder.”
In the 12 months prior to their first ketamine infusion, “patients had completed a mean of 39 mental health visits, 22% had received inpatient psychiatric treatment, 13% had received repetitive transcranial magnetic stimulation (rTMS) and 18% had received electroconvulsive therapy,” the study reported.
“Our study found that, after 6 weeks of treatment, 26% of the veterans with treatment-resistant depression improved their depression scores by 50%, and 15% of the veterans were in remission,” Pfeiffer said. “These improvements were sustained for at least six months with decreasing infusion frequency.”
“The patients who received ketamine for depression had highly treatment-resistant, moderately-severe depression with an average of six prior antidepressant medication trials and frequent use of outpatient mental health services. The vast majority of patients found the treatment acceptable, with 50% achieving clinically meaningful response and 15% achieving remission. These gains were maintained for at least six additional months with continued infusions,” he explained.
The authors found that intravenous ketamine treatment was “rarely used to treat depression in the VA in fiscal year 2020, with less than one-fifth of VAMCs administering the treatment and only 215 patients out of hundreds of thousands with depression receiving the treatment.”
Clinicians should consider “repeated IV ketamine infusions as a treatment option for patients who have failed multiple oral antidepressant medications, psychotherapy and/or repetitive transcranial magnetic stimulation (rTMS),” noted Avinash Hosanagar, MD, director of the neuromodulation clinic and a staff psychiatrist at LTC Charles S. Kettles VAMC at VA Ann Arbor Healthcare System.
“Patients who show improvement in their depression with an acute course of ketamine may benefit from continued infusions to maintain their gains from the initial course,” Hosanagar told U.S. Medicine. “While no specific clinical characteristics were identified in our study as predictors of response, our study did show that most veterans with high rates of antidepressant treatment failures and psychiatric comorbidity responded well to ketamine.”
The authors advised about some possible adverse effects of intravenous ketamine treatment.
“During any IV ketamine treatment, patients can experience adverse effects, such as heightened awareness of light and sounds, nausea, vomiting, headache, elevation in their blood pressure and a sense of dissociation from their body or their surroundings,” according to the study.
“Infrequently, it can cause changes in heart rate and rhythm. Most of these side effects subside within 1 to 2 hours of the infusion,” Hosanagar said. “Patients are advised not to drive for 24 hours after receiving ketamine. Rarely, and primarily when used outside of a treatment setting, it can cause urinary bladder and gastrointestinal dysfunction.”
- Pfeiffer PN, Geller J, Ganoczy D, Jagusch J, Carty et. Al. Clinical Outcomes of Intravenous Ketamine Treatment for Depression in the VA Health System. J Clin Psychiatry. 2024 Jan 8;85(1):23m14984. doi: 10.4088/JCP.23m14984. PMID: 38206011.