RAND: Not Enough information on Alternatives to Opioid Therapy
WASHINGTON — While it’s been long understood that servicemembers suffer from chronic pain at higher rates than their civilian counterparts, a new study by the RAND Corp. has found that a lack of administrative data and a dearth of research into treatments limits how successfully that pain can be treated.
Chronic pain is defined as pain that lasts for at least three months, and the prevalence of chronic pain in the military is estimated to be between 31% and 44%, much higher than the 20% in civilian adults. The most common pain etiology among servicemembers is musculoskeletal pain, particularly back and joint disorders, and chronic pain is more common for those injured in combat or exposed to high-intensity combat.
“Because of the unique occupational exposures associated with deployments … servicemembers are also at risk of more complex chronic pain syndromes,” the RAND report states. “For example, combat injuries, particularly blast injuries, can result in complex poly trauma, with a higher number, severity and diversity of wounds, and a high incidence of concurrent traumatic brain injury.”
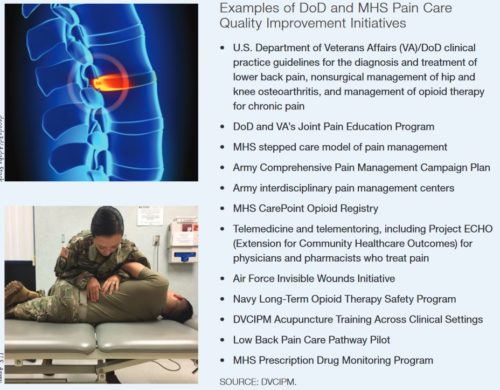
Over the last decade, DoD and MHS have become deeply invested in discovering new treatments for chronic pain, driven by increased awareness of the high prevalence the condition among servicemembers, as well as a growing understanding of the dangers of opioids. Recent studies have shown that, not only does opioid therapy under-perform in easing chronic pain in the long term, but the negative health consequences are considerable.
New treatment modalities include physical therapy, occupational therapy, chiropractic treatment, cognitive behavioral therapy and alternative therapies, such as acupuncture. On the pharmacological side, physicians are increasingly prescribing NSAIDs, anticonvulsants, antidepressants and muscle relaxants instead of opioids in an attempt to ease patients’ pain.
Despite investment into chronic pain treatment, significant knowledge gaps in just how successful those treatments are with servicemembers has hampered care. While MHS tracks some pain care metrics, RAND’s investigators found that limited published evidence on healthcare utilization or the quality of care received by servicemembers with chronic pain. Instead, most published studies have centered on the effects of opioids on pain management.
“One significant limitation is that administrative data only capture the use of health services that are covered, in whole or in part, by insurers,” the report explains. “This limitation is particularly relevant to research on chronic pain because several widely used pharmacologic pain treatments can be purchased over the counter (e.g., acetaminophen, NSAIDS) and therefore might not be associated with a prescription drug claim. Moreover, many popular complementary and alternative medicine treatments for chronic pain are not reimbursed by insurance.”
Consequently, administrative data might systematically underestimate the use of those therapies.
The report also found that administrative data contains little information about the content of medical counters beyond services that have been coded for insurance purposes. Useful information that would not be coded includes functional assessments and the specific behavioral therapies that have been delivered.
Another important gap in patient data is the frequent lack of patient-reported outcomes. These are critical when it comes to assessing pain severity and how the servicemember is responding to treatment.
This lack of understanding of the severity of servicemembers’ chronic pain could also have an effect on force readiness.
“The adverse effects of painful injuries on military readiness have been well documented, but these studies have not typically distinguished between the short-term effects of acute injuries and the long-term effects of chronic pain,” the report states. “Most research on the consequences of chronic pain in military populations has involved retrospective analyses of VA cohorts who are likely not representative of the population of servicemembers receiving care through the MHS. … However, the limited available evidence indicates that the effects of chronic pain on servicemembers’ readiness are likely substantial.”
Distinctive Features
The report pinpoints a number of ways that the MHS can improve its administrative data in order to gain a better understanding of chronic pain among servicemembers. The first is to better describe the distinctive features of a patient’s chronic pain. While many servicemembers have etiologies that resemble those found in civilian patients, there can be distinctive syndromes unique to military personnel. Rather than identify that a patient suffers from chronic pain using a single diagnostic code, clinicians might employ an approach that requires multiple diagnostic codes over a specified observational period. More complete data on the specifics of a patient’s chronic pain will provide MHS with a better understanding of their treatment progress.
Also, more research is needed on just which treatments are most effective so that they can be adopted more broadly.
“Although DoD and the military services internally track chronic pain care processes and assess quality, specific approaches to quality measurement may vary, and it is not always clear to what extent valid and reliable performance metrics are used,” the report notes.
By improving the data that goes into a patient’s record and optimizing the use of what’s already there, the report’s authors believe that MHS will be better positioned to evaluate effective pain treatments as well as to better identify servicemembers suffering from chronic pain who might otherwise go untreated.