ANN ARBOR, MI — Benzodiazepines, including alprazolam (Xanax) and clonazepam (Klonopin), are among the most commonly prescribed drugs for anxiety and sleep disorders. They also carry a significant risk of side effects.
For older people, in particular, they are known to impair cognition, mobility and driving skills and to increase the risk of falls. For that reason, decreasing benzodiazepine prescriptions has been a goal of the VA system and a success story since the VA Psychotropic Drug Safety Initiative (PDSI) was launched in 2013. The PDSI is a nationwide psychopharmacology quality improvement initiative designed to improve the safety and effectiveness of psychopharmacologic treatment.
But some centers within the VA system have done better than others, according to a new study, which provides insights for other centers and health systems working to decrease benzodiazepine prescriptions. 1
To better understand the magnitude of reductions in benzodiazepine prescriptions and strategies that have proven effective in achieving those reductions, researchers led by Donovan Maust, MD, associate director of the Geriatric Psychiatry Program and research scientist at the Ann Arbor, MI, VA Center for Clinical Management Research, used national VA data to look at benzodiazepine prescribing to older veterans.
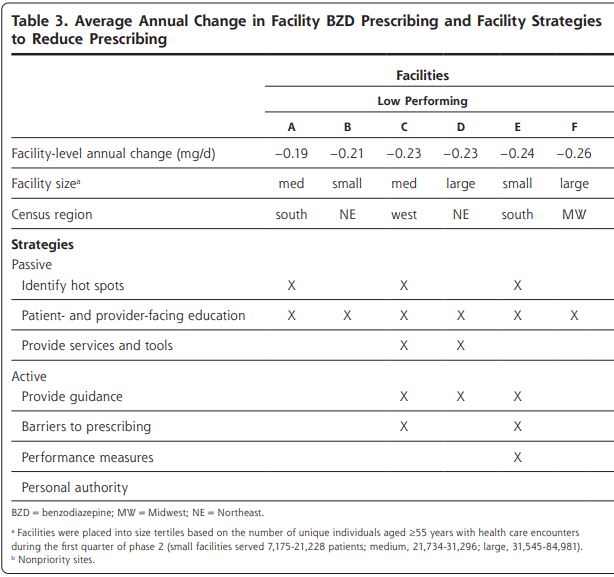
Among veterans aged 75 and older receiving long-term benzodiazepine treatment, the researchers stratified facilities into relatively high and low performance on the basis of the reduction in average daily dose of prescribed benzodiazepines from Oct. 1, 2015, to June 30, 2017. They then interviewed key facility personnel who led local benzodiazepine reduction efforts representing 11 high-performing and six low-performing facilities.
On the basis of the themes that emerged across facility interviews, the researchers sorted strategies centers used as passive or active. Passive strategies generally focused on enhancing knowledge, but were potentially easy for clinicians and patients to disregard. Active strategies were designed to counter prescribing inertia—a common barrier to deprescribing—and encourage clinicians to either deprescribe benzodiazepines or provide an explicit clinical rationale for why continued prescribing was appropriate. Whereas passive strategies were commonly used across all facilities, active strategies were more often found in high-performing facilities.
They found that all facilities interviewed—regardless of performance—used passive strategies, including education about appropriate prescribing, alternatives to benzodiazepines and the identification of potential patients for benzodiazepine discontinuation.
“At higher performing centers, however, clinicians provided more advice and help,” Maust told U.S. Medicine. “In particular, there were some facilities where chart reviews would happen, and the clinicians would give specific recommendations about how to manage their medications and possible alternative medications.
Clinical Pharmacists Help With Process
“Generally the more successful facilities had active involvement from clinical pharmacists who could help with the tapering process,” Maust continued. “Depending on the state and their licensing, they could either do the tapering themselves or provide recommendation back to the primary care clinician to do it. And finally the higher achieving facilities there was a personal authority—often a respected clinician colleague—who said ‘this is really important, this is the right thing to do for veterans, I strongly encourage you to do this, I am going to help you do this.’”
The important take home of the study is that “education is not enough,” Maust said. “It might make the people providing it feel better, but if they really want to improve prescribing, they have to do more than that”.
“When you look at trends in prescribing, over time it has been going down in the VA but not so much in the community,” he said. “[In the community], the vast majority of prescribing is by primary care clinicians, who are unbelievably overburdened with the amount of care that they need to provide. These are complex conversations and decisions needed, and primary care clinicians need help, and they really are not able to do this without support, so I think a system that wants to address benzo prescribing there needs to be a system to support primary care clinicians to do that.”
The authors concluded that the study provides important evidence suggesting that multicomponent interventions are necessary to support the difficult work of patient and clinician behavior change.
- Maust DT, Takamine L, Wiechers IR, Blow FC, Bohnert ASB, Strominger J, Min L, Krein SL. Strategies Associated With Reducing Benzodiazepine Prescribing to Older Adults: A Mixed Methods Study. Ann Fam Med. 2022 Jul-Aug;20(4):328-335. doi: 10.1370/afm.2825. PMID: 35879067; PMCID: PMC9328717.