EL PASO, TX — A significant number of servicemembers deployed to southwest Asia report an increase in respiratory symptoms during and after their tours of duty, but epidemiological data have not demonstrated an increase in diagnoses of asthma or other respiratory illnesses. Whether deployment to Iraq or Afghanistan worsened existing asthma has remained an open question as well, until now.
In the United States, one in 12 people currently suffers from asthma, with higher rates seen among African Americans. While active asthma precludes military accession, individuals who have not experienced asthma symptoms since their 13th birthday are no longer precluded from joining the military. In some instances, the various challenges posed by service may reactivate childhood asthma. In addition, individuals who develop asthma while on active duty may stay in the service, if it remains under control, so understanding the impact of deployment on respiratory health has become increasingly important.
Many studies have examined the environmental conditions in Iraq and Afghanistan to better assess the risk of respiratory illnesses. The region has a great deal of geological dust and some locations experience high levels of vehicle exhaust and industrial air pollution. Military bases in the area also used burn pits to dispose of waste materials of all kinds, contributing to the existing environmental exposures.
A number of studies have examined aspects of the relationship between asthma and deployment. As previously reported in U.S. Medicine, deployment to southwest Asia itself does not appear to increase the risk of new-onset asthma, though combat likely does.1 An earlier retrospective case-control study of 400 servicemembers who were evaluated for fitness for duty related to asthma that compared deployed to nondeployed personnel found no difference in spirometry between the deployed and nondeployed groups. Further, it demonstrated no difference in spirometry or asthma severity classification among those diagnosed with asthma before or after deployment.2
More recent research sought to conduct a more direct assessment of the respiratory effects of deployment on asthmatics. To conduct the study, physicians in the pulmonary/critical service, department of medicine, at the William Beaumont Army Medical Center in El Paso and the Brooke Army Medical Center at Fort Sam Houston, Texas, examined the health records of 642 active duty servicemembers with asthma. All had a documented diagnosis and spirometry measures on file and deployed to southwest Asia between 2006 and 2015.3
Undiagnosed predeployment lung disease and a lack of objective data could be significant confounding factors in such a study, particularly given that deployed servicemembers are older, heavier and more likely to smoke than those who do not deploy.4 Consequently, the team chose to analyze the subset of 76 individuals who had spirometry assessments both before and after deployment.
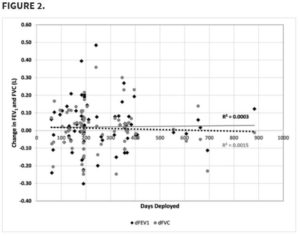
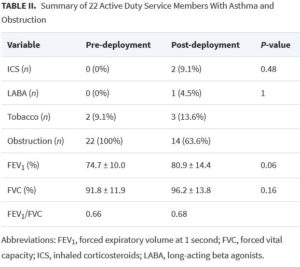
The researchers found no significant change in post-deployment forced vital capacity (FEV), forced expiratory volume at one second (FEV1) or in the use of inhaled corticosteroids or long-acting beta agonists. Tobacco use and mean body mass index also did not vary significantly.
Two subgroups—tobacco users and those with spirometric obstruction prior to deployment—also showed no decline in FEV or FEV1. Perhaps counterintuitively, individuals with predeployment spirometric obstruction demonstrated improved FEV1, though the 6.2 increase in percent predicted was not significant.
“Our observed trend to improve post-deployment FEV1 in the asthmatic population with predeployment obstruction cannot be easily explained as an effect of deployment, but its presence does suggest that deployment is not associated with any deleterious effect on postdeployment spirometric measures of lung function in this population,” the researchers said.
That finding echoed a post-deployment nonsignificant improvement in FEV1 and FEV seen in the STAMPEDE II study of 843 soldiers with and without asthma who departed from Fort Hood, TX, to southwest Asia, they noted. “Predeployment testing with spirometry and impulse oscillometry was unable to detect any significant change,” the STAMPEDE II researchers said. “In those with abnormal spirometry predeployment or asthma history, there was also not identifiable change that indicated worsening lung function.” 5
Looking at the two studies together provides some reassurance. “Although baseline lung function is lower in the asthmatic population we studied (FEV1 86.0% predicted), when compared with the general population (FEV1 95.2% predicted) of the Study of Active Military Personnel for Pulmonary Disease Related to Environmental Deployment Exposure II trial, a nonsignificant increase in FEV1 and FVC is seen in both populations,” the Beaumont-Brooke team wrote. “These data sets both provide evidence that there is no measurable effect of deployment on post-deployment spirometric measures of lung function, even among military personnel with existing asthma and reduced baseline spirometry.”
- Rivera AC, Powell TM, Boyko EJ, Lee RU, Faix DJ, Luxton DD, Rull RP; Millennium Cohort Study Team. New-Onset Asthma and Combat Deployment: Findings From the Millennium Cohort Study. Am J Epidemiol. 2018 Oct 1;187(10):2136-2144.
- DelVecchio SP, Collen JF, Zacher LL, Morris MJ. The impact of combat deployment on asthma diagnosis and severity. J Asthma. 2015 May;52(4):363-9. doi: 10.3109/02770903.2014.973502. Epub 2014 Oct 22. PMID: 25290816.
- Woods JT, Walter RJ, Houle MC, Barber BS, Morris MJ. The Effect of Deployment on Pulmonary Function in Military Personnel With Asthma. Mil Med. 2020 Dec 21:usaa558. doi: 10.1093/milmed/usaa558. Epub ahead of print. PMID: 33346840.
- Skabelund AJ, Rawlins FA 3rd, McCann ET, Lospinoso JA, Burroughs L, Gallup RA, Morris MJ. Pulmonary Function and Respiratory Health of Military Personnel Before Southwest Asia Deployment. Respir Care. 2017 Sep;62(9):1148-1155. doi: 10.4187/respcare.05438. Epub 2017 May 2. PMID: 28465382.
- Morris MJ, Skabelund AJ, Rawlins FA 3rd, Gallup RA, Aden JK, Holley AB. Study of Active Duty Military Personnel for Environmental Deployment Exposures: Pre- and Post-Deployment Spirometry (STAMPEDE II). Respir Care. 2019 May;64(5):536-544. doi: 10.4187/respcare.06396. Epub 2019 Jan 8. PMID: 30622173.