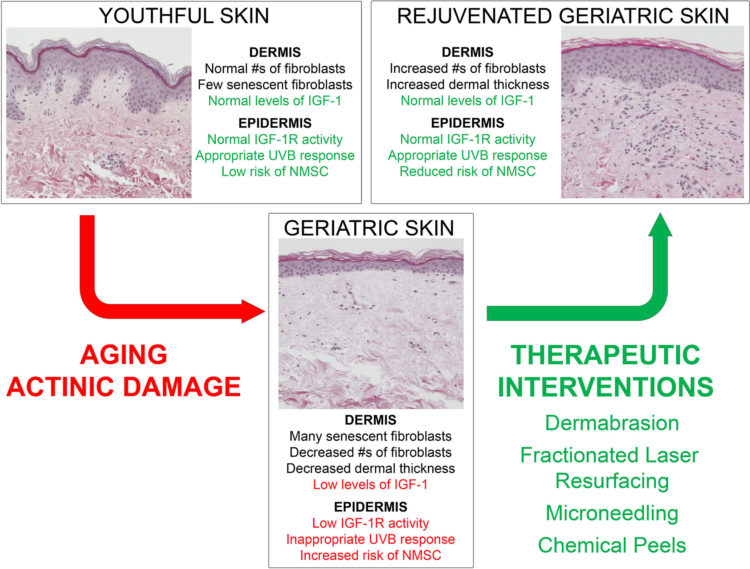
Click To Enlarge: Model demonstrating young versus aged skin and the impact of wounding therapies on the response of geriatric skin to UVB-irradiation.
DAYTON, OH — The most common form of cancer, nonmelanoma skin cancer (NMSC) — composed primarily of basal cell carcinoma and squamous cell carcinoma — affects about 3.3 million people annually. The occurrence of skin cancer substantially increases with age, thus is a concern for the aging veteran population, many of whom also experienced high cumulative sun exposure during active duty.
Although NMSC rarely metastasizes, it can spread locally, potentially damaging surrounding tissue and underlying bone, and it often recurs after treatment. Surgery is the most common treatment. Other forms of treatment include physical destruction (cryotherapy, radiotherapy, and curettage and cautery), chemical destruction (photodynamic therapy), local therapies (topical 5-fluorouracil, imiquimod, ingenol mebutate and diclofenac), and novel hedgehog pathway inhibitors (HPI) (vismodegib and sonidegib).
Prevention has traditionally focused on the use of sunscreens and protective clothing; however, collaborative research teams led by VA researchers Jeffrey Travers, MD, and Dan Spandau, PhD, are beginning to apply a new understanding of the mechanisms which lead to the development of skin cancer into treatments that show promise for preventing its occurrence.
Understanding the Cause
Aging and excessive UV exposure have long been recognized as the greatest risk factors for NMSC development. However, the exact mechanisms by which aging and sunlight exposure led to the development of cancer was not well understood.
Findings in recent years by Spandau, an associate research professor of dermatology at the Indiana School of Medicine, and Travers, professor of dermatology at Boonshoft School of Medicine at Wright State University and staff physician at the Dayton, OH, VAMC, have implicated the significance of the insulin-like growth factor-1/insulin-like growth factor-1 receptor (IGF-1/IGF-1R) pathway in the development of NMSC.
Prior research had shown that the intensity of UVB exposure directly correlates with the extent of DNA damage. Additionally, it has been shown that the regulation between IGF-1/IGF-1R is vital in the protective response and indicative of the tendency for photocarcinogenesis. Adequate IGF-1 production in dermal fibroblasts is necessary for the appropriate epidermal keratinocyte response to UVB-damaged DNA. Geriatric skin exhibits suppressed IGF-1 signaling due to an increased cellular senescence profile of fibroblasts. This allows UVB-induced DNA damage to proliferate unchecked, which increases the likelihood of malignant transformation.
Thus, the researchers reasoned, the IGF-1/IGF-1R signaling pathway could be exploited for therapy; they theorized that wounding therapy might be a way to do so. By inducing a “wounding response,” these therapies, which were developed for cosmetic applications, attempt to reverse the geriatric fibroblast senescence phenotype.
Promise for Prevention
Spandau and Travers tested this theory using fractionated laser resurfacing (FLR), a technique which delivers infrared light to tissue where it is absorbed by water in the dermis, causing skin heating at non-ablative wavelengths vaporization of tissue layers at ablative wavelengths which induces skin wounds, said Spandau, who is affiliated with the Richard Roudebush VAMC in Indianapolis. “Importantly, this technique spares islands of normal skin, which can facilitate the healing process.”
Researchers performed FLR on one arm of geriatric veterans from the Dayton VAMC and compared the development of NMSC (as well as the NMSC precursor lesions called actinic keratosis, AK) on the FLR-treated arm to the untreated arms. Veterans were examined every six months following FLR treatment, and the number of AKs and NMSCs were mapped and recorded for each arm. “After three years, FLR treatment led to a remarkable 92% reduction in the occurrence of NMSC,” said Spandau. “Importantly, our data indicated that FLR treatment was actually preventing the development of new skin cancers.” 1
Findings from FLR research led the researchers to examine the potential effectiveness of other—more accessible and less expensive —wounding therapies, including microneedling and chemical peels, against NMSC development. Microneedling is a reasonably new treatment modality within the field of dermatology that involves pricking the skin with tiny sterilized needles. Chemical peeling utilizes a chemical application to the skin that causes controlled wounding of the epidermis and dermis, resulting in skin regeneration. The extent of wounding depends on the depth of skin penetration, said Spandau, adding that a number of human studies suggest chemical resurfacing may be a viable skin cancer prophylaxis.
A review of those therapies published Jan. 7 in Frontiers in Oncology showed promise for both therapies. 2
Microneedling: In the review, nine geriatric volunteers with Fitzpatrick Types I and II underwent wounding on the upper buttocks using a commercially available microneedling device. After 90 days, a localized area of either microneedle-treated skin or untreated skin was irradiated with a dose of UVB At three months after microneedling application, punch biopsies revealed mRNA levels of both collagen 1 and IGF-1 were increased in previously wounded skin. Furthermore, this response to UVB irradiation was similar to the “normal” responses documented in young skin, indicating that wounding of geriatric skin by use of a microneedling device results in increased dermal collagen 1 and IGF-1 levels as well as normalizes the protective response to UVB irradiation. The authors said the findings are promising but are limited to a short time frame and small sample size.
Chemical peels: The groups’ early preliminary studies exploring trichloroacetic acid (TCA) peels as a potential treatment for treating actinic keratosis AKs indicate that a 10% TCA peel on geriatric skin upregulates IGF-1 mRNA levels approximately two-fold at 90 days. “As presented, chemical peeling holds promise as a therapeutic and preventative modality for skin carcinogenesis,” the authors wrote, noting more research is needed with this area to elucidate the precise mechanize of skin rejuvenation.
Based on the new understanding of mechanisms in skin cancer development, wounding therapies hold promise as evidenced by their ability to restore appropriate IGF-1/IGF-1R signaling to levels found in younger skin, the authors concluded. “The concept of restoring youth and combating malignancy through wounding therapies holds potential as a major dermatological treatment modality,” they wrote, noting that further translational research is needed to explicate the direct pathways by which they are able to rejuvenate geriatric skin and prevent malignant transformation.
- Spandau DF, Chen R, Wargo JJ, et al. Randomized controlled trial of fractionated laser resurfacing on aged skin as prophylaxis against actinic neoplasia. The Journal of Clinical Investigation. Published August 24, 2021. https://doi.org/10.1172/JCI150972
- Frommeyer TC, Rohan CA, Spandau DF, Kemp MG, Wanner MA, Tanzi E, Travers JB. Wounding Therapies for Prevention of Photocarcinogenesis. Frontiers in Oncology. Published online January 7, 2022. doi: 10.3389/fonc.2021.813132

