New Study Assesses the Shift; Telemedicine Here to Stay
MENLO PARK, CA — Like other healthcare systems, the VHA has faced unprecedented challenges in responding to the COVID-19 pandemic. A new study provides a broad look at how VA care patterns have shifted since the start of the pandemic.
“We wanted to know not just how much telehealth the VA was providing but also how much care it was purchasing in the community,” said the study’s lead author, Liam Rose, PhD, a health economist with the VA Palo Alto Health Care System in Menlo Park, CA.
Rose said he knew a portion of the shift in care was due directly to the pandemic but suspected some also was likely due to the VA Mission Act of 2018. Implemented less than a year before the beginning of the pandemic, the act made the VA both a provider of care and a payer of care in the community (community care), Rose said. “So we were kind of getting a trend of both things at once to see how it was going.”
For the cross-sectional study, Rose and his colleagues extracted records from the VA’s Corporate Data Warehouse on all healthcare encounters purchased or provided by the VHA from Jan. 1, 2019, to March 28, 2021. Encounters were then classified into mutually exclusive categories by location (VHA and community care) and type of care delivered (inpatient, emergency department, urgent care and outpatient).1
Decrease in Visits
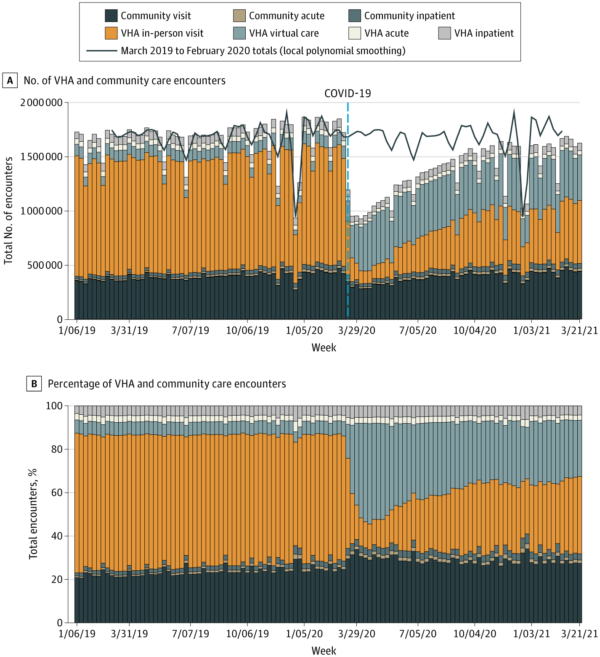
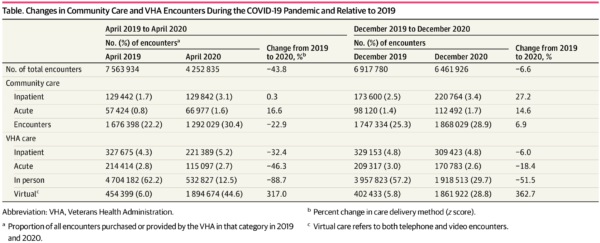
Click To Enlarge: Numbers (A) and percentages (B) of all health care encounters purchased (community care) or provided by the US Veterans Health Administration (VHA). Acute care refers to inpatient, emergency department, and urgent care encounters. Virtual care refers to both telephone and video encounters.
As expected, the study found that overall health care use decreased substantially in March and April 2020—1.97 million encounters in the last week of February 2020 vs. 1 million in the first week of April 2020. Strikingly, the number of total encounters had not yet recovered to pre-pandemic levels, which was 1.97 million encounters per week in February 2020 vs 1.7 million per week in February 2021. The estimated total number of missing encounters relative to the previous year was 16.5 million.
Other key findings:
- Virtual care quickly expanded (90,400 encounters in the last week of February 2020 vs. 404,000 encounters in the first week of April 2020).
- The number of VHA virtual care encounters increased from 454,399 (6.0%) in April 2019 to 1,894,674 (44.6%) in April 2020, then decreased to 1,861,922 (28.8%) in December 2020.
- The number of nonacute community care encounters was 1,676,398 (22.2%) in April 2019 compared with 1,292,029 (30.4%) in April 2020 but had increased to beyond the pre-pandemic number (1,868,029 [28.9%]) as of December 2020.
“In short, virtual care went way up and stayed way up. Community care is a much larger portion of what the VA is doing than it used to, and in-person is way down even a year into the pandemic,” Rose told U.S. Medicine.
He said it’s possible that the higher utilization of community was unrelated to the pandemic. “If there was no COVID, perhaps the VA would have the same issue because of the Mission Act and the VA becoming more of a payer, but I can’t say with certainty,” he said. “Another possible explanation is that community providers may have been quicker to return to in-person care than the VA, which didn’t the face the same financial incentives.”
One thing Rose can say with near certainty is that virtual care is here to stay. “The VA has always been a leader in virtual health and perhaps that is how it will continue to go,” he said.
The study’s results indicated that existing trends pushing the VHA toward being a mixed payer and provider may have been accelerated, a situation that warrants more consideration, Rose said.
“VA and Congress will have to think about the right mix between being a payer, which often grants good access to people who are not close to a VA facility, and being a provider, where they are very good at taking care of veteran-specific issues within the VA.”
- Rose L, Tran LD, Asch SM, Vashi A. Assessment of Changes in US Veterans Health Administration Care Delivery Methods During the COVID-19 Pandemic. JAMA Netw Open. 2021;4(10): e2129139. doi:10.1001/jamanetworkopen.2021.29139