Reasons Include Depression Diagnoses, Dual Healthcare
CHARLESTON, SC — Cardiovascular disease is the No. 1 cause of death for women in the United States, and female veterans are at particular risk. Female veterans experience higher rates of cardiac death than civilian women and exhibit high rates of known cardiovascular disease risk factors, including diabetes and depression.1
Still, research has shown that women, including women veterans, receive suboptimal heart care compared to men. Clinical guidelines recommend statin therapy for nearly all patients with diabetes to prevent cardiovascular disease, regardless of sex or LDL cholesterol levels. Yet women who are eligible for this therapy are less likely than men to be treated with cholesterol-lowering statins or to be prescribed a statin at the appropriate intensity—a disparity that has also been documented within the VA healthcare system.
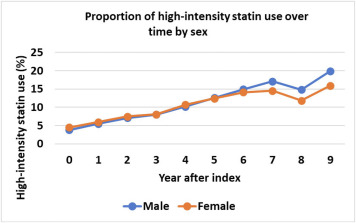
A new nationwide study published in Women’s Health Issues sheds more light on the factors contributing to sex disparities in statin use among veterans with diabetes.2 The research team analyzed health records—including data from the VHA and Medicare/Medicaid—of more than 714,000 older veterans with Type 2 diabetes, including 9,600 women. They examined associations between sex and statin use while adjusting for several covariates, including proxies for subjects’ access to care. Their findings demonstrate that women veterans continue to be undertreated with statin therapy for cardiovascular disease prevention and that a great deal of this disparity is related to access to care and mental health conditions.
“The details of comorbidities and proxies for use and access to care allowed for a more comprehensive assessment of potential factors causing this disparity, which are important if interventions to address these issues are to be developed and tested,” said Casey Buchanan, Ph.D. a research scientist at the Charleston Health Equity and Rural Outreach Innovation Center (HEROIC) at Ralph H. Johnson VAMC and the paper’s lead author.
In the base model analysis of odds of any statin use (which included only sex and the number of years the patient was seen in the VA medical records), women veterans were 14% less likely to be using statins than men. After adjusting for demographic measures (such as race/ethnicity, age, marital status, and location of residence) and clinical variables (such as smoking status and atherosclerotic cardiovascular disease), women were 8% less likely to be using any statin compared to men. After controlling for dual use of both the VA healthcare system and Medicare, women were 6% less likely to receive statins than men. (Dual healthcare use—using services from VHA and non-VHA organizations—is increasing among veterans and has been associated with suboptimal outcomes, Buchanan said.)
Less Disparity
In the fully adjusted model, which controlled for subjects’ service-connected disability rating (an assessment of medical conditions connected to military service—a rating that affects patients’ healthcare access and costs), number of primary care visits, and mental health comorbidities, the disparity shrank to 3%.
“Including markers of access to VA care (service-connected disability rating, dual use status, and primary care visits) and mental health comorbidities in our fully adjusted model greatly narrowed the observed sex disparity in statin therapy among our sample of older veterans with diabetes and the disparity lost statistical significance,” Buchanan told U.S. Medicine.
For example, Buchanan noted, service-connected disability rating is a strong predictor of access to and use of the VA healthcare system. (Veterans with higher disability ratings receive priority VA care, and veterans with disability ratings of 50% or more are exempt from prescription co-payments.) The study found that more men than women had service-connected disability ratings of 50% or higher—a rating that also was associated with 36% higher odds of statin use.
Conversely, history of a psychiatric disorder and depression were associated with lower odds of statin use. Depression is common among patients at high risk for cardiovascular disease, and there is evidence that female veterans are more likely to be diagnosed with depression or PTSD compared to both male veterans and civilian women. Depression also is thought to contribute to poor adherence to medications, including statins and blood pressure lowering medications.
“This may deter a provider from initiating statin therapy with a patient with these comorbidities or poor adherence may influence a provider to discontinue statin therapy,” Buchanan explained.
The study notes that other health system factors—such as fragmentation of care, as observed in subjects’ dual use of the VA and Medicare—may also contribute to sex disparities in statin use. The researchers found that in the fully-adjusted model for the outcome of any statin use, subjects with less than 50 percent VHA use had 77 percent lower odds of receiving any statin therapy compared to subjects with 80 percent or more VHA use.
While dual healthcare use increases care options for veterans, it also increases the potential for fragmented care. This is true for both male and female veterans; however, the VA has historically lacked sex-specific health services for women veterans, and as a result they are more likely than men to see multiple providers in multiple sites.
“The VA has achieved significant improvements in women’s primary care and in reducing sex disparities for many clinical prevention measures and now often outperforms many private sector quality metrics, like breast cancer screening, for example,” said Buchanan. “However, there is still more work to be done closing the gaps in areas like diabetes and lipid control.”
- Ebrahimi, Ramin, et al. Trends in Cardiovascular Death Rates Among Women Veterans. American Heart Association’s Scientific Sessions 2021.
- Buchanan, Casey H., Brown, Elizabeth A., Bishu, Kinfe G., Weeda, Erin, et al. The Magnitude and Potential Causes of Sex Disparities in Statin Therapy in Veterans with Type 2 Diabetes: A 10-year Nationwide Longitudinal Cohort Study. Women’s Health Issues. Published December 20, 2021. DOI: 10.1016/j.whi.2021.10.003.