Variations Underscores Importance of Surveillance at VA
 NEW YORK — If you think of a patient at risk for hepatitis C infection (HCV), a man likely comes to mind, and for good reason. HCV occurs in men at four times the rate it does in women.
NEW YORK — If you think of a patient at risk for hepatitis C infection (HCV), a man likely comes to mind, and for good reason. HCV occurs in men at four times the rate it does in women.
For years, HCV has driven the number of cases of hepatocellular carcinoma (HCC) seen at the VA, with the same 4:1 ratio persisting from chronic infection to malignancy. With the virtual elimination of HCV in the VA in the last seven years, researchers have started to look at other risk factors and the impact they have on the VA’s advanced liver disease (ALD) program.
One fact has united much of that research: almost all types of liver disease develop and progress very differently in women than in men. While women have a lower risk of HCV-related HCC, they have a higher risk for HCC arising from other causes. As a result, surveillance programs designed to pick up HCV patients at greatest risk of developing HCC may miss female veterans.
Those programs largely track the typical progression in men from HCV to HCC. Between 15% and 25% of men infected with hepatitis C will spontaneously clear the infection. Of the 75% to 85% who develop chronic hepatitis, 10% to 20% will develop cirrhosis and 1% to 4% will eventually develop hepatocellular carcinoma.1
In contrast, women are more than twice as likely to spontaneously clear HCV infections, with reported rates from 34% to 45%. They are less likely to progress to severe liver disease, with 27% developing fibrosis and just 2% progressing to cirrhosis.2
The lower rate of HCV-related cirrhosis does not mean women do not develop HCC. In a recent article in the American Journal of Gastroenterology, researchers at Columbia University, the Richard L. Roudebush and Bronx VAMCs, and their colleagues found that “there were important differences in the underlying etiology of liver disease between the two genders (P<0.0001).”3
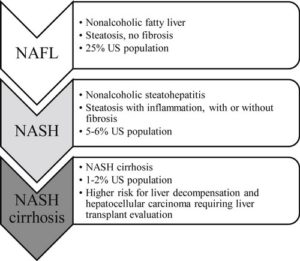
The study analyzed data from 5,327 patients treated for HCC in five large centers between January 2000 and June 2014, of which 1,203 self-identified as women. While women were twice as likely to have nonalcoholic fatty liver disease (NAFLD) as men (23% vs. 12%), they developed alcoholic liver disease at one-third the rate (5% vs. 15%).
With alcohol- and HCV-related HCC, patients typically progress to fibrosis and then cirrhosis, whereas with hepatitis B, HCC can occur in a completely non-fibrotic liver. In the study, they sought to determine whether NAFLD progressed more like HCV and alcohol or hepatitis B. Notably, the researchers found that noncirrhotic HCC was much more prevalent in women than in men (17.1% vs. 9.7%).
“The area of interest that we found to warrant further exploration is particularly with regards to non-alcoholic steatohepatitis (NASH),” said corresponding author Julia Wattacheril MD, MPH, director, Nonalcoholic Fatty Liver Disease Program, Center for Liver Disease and Transplantation, Columbia University Irving Medical Center in New York.
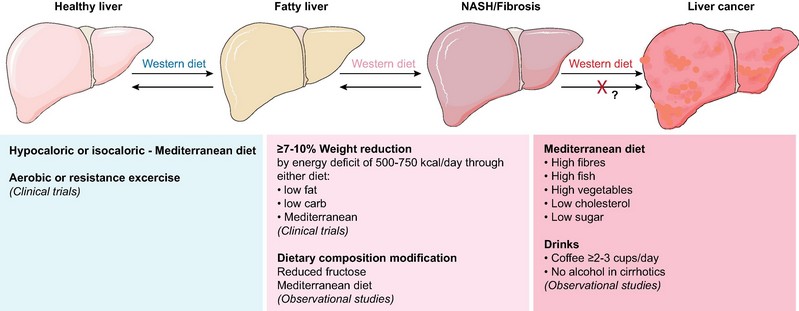
NAFLD is characterized by a fat build up in the liver. NASH is an advanced form of NAFLD that includes inflammation and liver damage as well as fat in the liver.
“Typically, when we study both fatty liver disease and cancer development within the context of fatty liver disease, we think that there’s a quote-unquote ‘protective effect of estrogen,’” Wattacheril told U.S. Medicine. Consistent with other data, she speculated that postmenopausal women could have an increased risk of disease, but the team did not specifically gather or analyze data on menopausal status for their study.
“We are starting to see evidence of HCC developing in precirrhotic tissue, typically we think of it being in individuals with advanced fibrosis (F3),” Wattacheril added. “Have we seen it in steatofibrosis, where it’s an early stage? Yes, on the case reportable level,” but larger studies will need to be done to understand its frequency and significance.
Some possible explanations for the differences in progression to HCC between women and men could be attributed to variation in peripheral adiposity, muscle metabolism differences, and fat distribution inside and outside of the liver, Wattacheril noted, but larger, prospective, longitudinal studies are required to tease out the roles those factors and other play in HCC development.
“The VA has a perfect patient population and a perfect system to be able to study some of these longitudinal effects because screening and surveillance can be rather systematic among that population, so I look forward to seeing some of the Veterans Affairs institutions studying this further,” said Wattacheril, who trained at the VA.
In the meantime, her research will focus on the metabolic milieu in which liver cancer develops and creating predictive models that could alert physicians that a patient has a high probability for having advanced fibrosis and should be considered for screening and cancer surveillance. “One of the reasons I love the VA system is you don’t have to worry about insurance coverage or clutter,” she said, “so that’s one of the most robust systems where you could do something like this.”
The VA has a vested interest in gaining greater understanding of the differences between men and women in development of HCC and liver disease more generally as the number of women serving in the military and the number of female veterans continues to rise.
“As we’ve become aware, we know so little about the differences between men and women and metabolizing medications or developing diseases,” Wattacheril concluded. “In so many ways, we’ve just assumed it must happen the same way it does in men. We were wrong so often, a lot of data needs to be basically rescinded and redone.”
- Axley P, Ahmed Z, Ravi S, Singal AK. Hepatitis C Virus and Hepatocellular Carcinoma: A Narrative Review. J Clin Transl Hepatol. 2018;6(1):79-84. doi:10.14218/JCTH.2017.00067
- Guy J, Peters MG. Liver disease in women: the influence of gender on epidemiology, natural history, and patient outcomes. Gastroenterol Hepatol (N Y). 2013;9(10):633-639.
- Phipps M, Livanos A, Guo A, Pomenti S, Yeh J, Dakhoul L, Burney H, Kettler C, Liu H, Miller E, Gawrieh S, deLemos A, Scanga A, Chalasani N, Wattacheril J. Gender Matters: Characteristics of Hepatocellular Carcinoma in Women From a Large, Multicenter Study in the United States. Am J Gastroenterol. 2020 Sep;115(9):1486-1495. doi: 10.14309/ajg.0000000000000643. PMID: 32453046.