
Marin Schweizer, PhD, Research Health Scientist Middleton VAMC and Professor of Infectious Diseases University of Wisconsin-Madison
MADISON, WI — Clinical decisions in the VA about whether to administer suppressive antibiotic therapy for patients with prosthetic-joint infections are often emotionally charged due to limited evidence about benefits and risks and potential consequences such as reinfection or amputation, according to a recent study.
The qualitative study published in JAMA Network Open examined how clinicians make decisions about suppressive antibiotic therapy for patients who had prosthetic-joint infections when there is limited evidence about benefits and risks. It also identified intervention opportunities to stop or reduce suppressive antibiotic therapy for patients who might not benefit.1
Prosthetic-joint infections after hip, knee or shoulder replacement surgery can have profound health effects. Suppressive antibiotic therapy is often prescribed after initial antibiotic treatment for prosthetic-joint infection, but there’s limited evidence on outcomes after this therapy.
Using suppressive antibiotic therapy for low-risk patients who might not need it could be associated with antibiotic resistance and adverse events, such as Clostridioides difficile infection. Either not prescribing or reducing length of suppressive antibiotic therapy for patients at low risk of prosthetic-joint infections may reduce the emergence of antibiotic-resistant organisms and the risks associated with long-term antibiotics, explained the lead investigators from the William S. Middleton Memorial Veterans Hospital and Clinics in Madison, WI, and colleagues.
Other researchers were from the Iowa City, IA, VA Healthcare System, the University of Iowa in Iowa City, IA, and the University of Wisconsin-Madison.
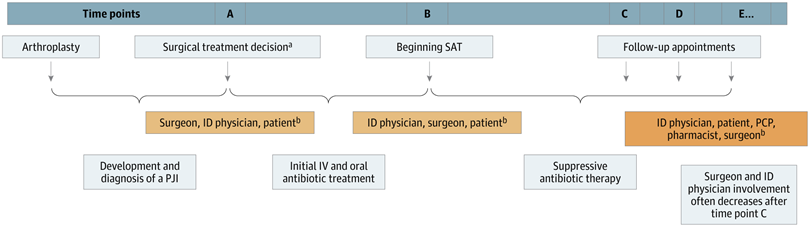
Click to Enlarge: ID indicates infectious diseases; IV, intravenous; and PCP, primary care physician.
a. Such as debridement, 1- or 2-stage exchange, or no surgery.
b. Degree of collaboration varies and may include others. Source: JAMA Network Open
In this study, the researchers interviewed 41 clinicians at eight VA hospitals who were involved in decision-making about suppressive antibiotic therapy after prosthetic-joint infection from Nov. 1, 2019, to July 31, 2021. The participating hospitals operated in seven states and represented 6 of the VA’s 18 regional Veterans Integrated Service Networks across the Southeast, Southwest, Middle Atlantic and Midwest. Analyses were completed between June 9, 2020, and Aug. 31, 2022.
Of the 93 VA hospitals that treat patients with prosthetic-joint infection, the authors said they wanted to maximize variability in suppressive antibiotic therapy treatment practices, so they selected facilities based on factors such as number of debridement vs. two-stage procedures after prosthetic-joint infection and days of antibiotic treatment. They also considered other hospital characteristics, such as region, patient volume, hospital complexity and presence of infectious diseases physicians.
Then, the researchers asked hospitals to identify orthopedic surgeons, infectious diseases physicians, advanced practice clinicians, nurses or case managers who were involved with suppressive antibiotic therapy prescribing after prosthetic-joint infection, as well as other individuals who made suppressive antibiotic therapy prescribing decisions or contributed information to help make those decisions, the study reported.
‘Emotionally Charged’
“Decisions about whether a patient receives suppressive antibiotic therapy were emotionally charged because of the limited evidence and potential for a reinfection and subsequent consequences such as amputation,” Marin Schweizer, PhD, a research health scientist at the Middleton VAMC and professor of infectious diseases at the University of Wisconsin-Madison, told U.S. Medicine.
“We found that suppressive antibiotic therapy decision-making could be a long process with multiple opportunities for decisions, rather than a one-time decision,” Schweizer explained. “At the first time point, surgeons determine whether a patient is eligible for revision surgery. Patients with limited surgical options are often given more suppressive antibiotic therapy. At the second time point, surgeons or infectious disease physicians make the initial decisions about suppressive antibiotic therapy. At some hospitals, surgeons took the lead; at others, infectious disease physicians took the lead, or surgeons and infectious disease physicians collaborated closely.
“Once the initial suppressive antibiotic therapy decision is made, primary care doctors, pharmacists and, of course, veterans themselves play critical roles. There were multiple times when all these key partners could decide whether to start or stop suppressive antibiotic therapy.”
When the research team began this study, investigators were focused on identifying a single decision point to prescribe suppressive antibiotic therapy after initial antibiotic treatment for the prosthetic-joint infection, she pointed out.
“Instead, we learned from interviewees that, while there was one point at which the primary suppressive antibiotic therapy prescribing decision was made, many other time points were associated with the decision,” Schweizer advised. “Also, different healthcare professionals were involved as decision-makers at different time points, sometimes without clear hand-offs. This provides multiple opportunities for shared decision-making to discuss benefits and risks of long-term antibiotics with patients.”
The study identified multiple potential decisionmakers for patients with prosthetic joint infections, including patients, surgeons, infectious disease clinicians, primary care practitioners and pharmacists.
“We also found significant time points that occur before or after the suppressive antibiotic therapy prescribing decision, including prosthetic-joint infection treatment decisions and follow-up appointments,” Schweizer noted. “We recommend shared decision-making conversations with the patients and antibiotic stewardship interventions to optimize the use of these long-term antibiotics. These conversations and interventions can be performed at multiple time points.”
She emphasized the importance of hand-offs from surgery or the infectious disease clinic to primary care practitioners.
“Often, primary care practitioners are being tasked with making later decisions about whether to stop or continue suppressive antibiotic therapy without good communication from the original prescriber about the goals of that antibiotic,” Schweizer said.
- Dukes KC, Walhof JF, Hockett Sherlock S, Suh D, et. Al. Decisions About Suppressive Antibiotics Among Clinicians at Veterans Affairs Hospitals After Prosthetic Joint Infection. JAMA Netw Open. 2025 Mar 3;8(3):e251152. doi: 10.1001/jamanetworkopen.2025.1152. PMID: 40105839; PMCID: PMC11923720.

