BALTIMORE, MD — An estimated one million people in the U.S. live with multiple sclerosis (MS) today, making understanding the economic impact of the disease a matter of increasing importance.
More than 28,000 veterans receive a diagnosis of MS annually, a number that has risen sharply in recent years. The incidence of the disease among veterans rose from 141 per 100,000 veterans in 1999 to 262 veterans per 100,000 in 2014. With such high and rising numbers of affected veterans, it is little surprise that the VA has been in the forefront of research on the cost of care and identification of the most effective therapies based on expanding knowledge of the pathophysiology of MS.
MS commonly strikes individuals between the ages of 20 and 40 and, for those serving in the military, it often represents a career-ending diagnosis. MS can affect mobility, social interactions, independence, memory and cognitive function, with substantial interpersonal variation in symptoms. For the 85% of patients with relapsing-remitting MS (RRMS), symptoms may wax and wane over time as well. The 15% with primary progressive MS (PPMS) may have plateau periods, but seldom have the remissions seen in RRMS.
Economic Burden
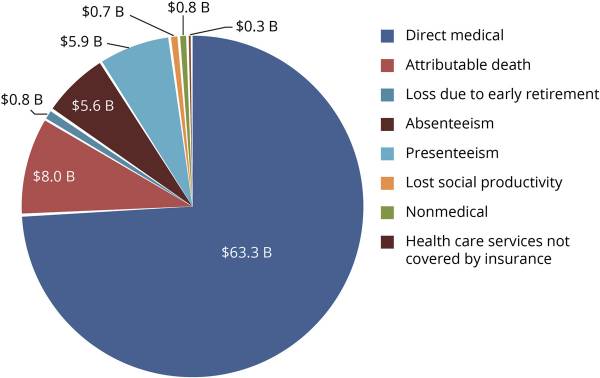
Researchers with the National Multiple Sclerosis Society, The Lewin Group, and Mitchell Wallin, MD, MPH, a neurologist with the VA’s Multiple Sclerosis Centers of Excellence, professor of Neurology and Rehabilitation Medicine at University of Maryland and George Washington University, recently estimated that the total economic burden of MS on the U.S. was $85.4 billion per annum. Direct medical costs account for $63.3 billion, with the balance incurred in indirect and nonmedical costs.1
“MS is a costly chronic disease, with direct costs of prescription drugs and indirect productivity loss being important cost drivers,” the authors said.
Overall, retail prescription medicine represented 54% of direct costs, with the cost of drugs administered in clinics accounting for another 12% and outpatient care 9%. On a per-person basis, the average excess medical costs exceeded $65,612 with more than half ($35,154) attributed to disease-modifying therapies (DMTs). Indirect costs on a per-person basis, including caregiving costs, averaged $22,875. The largest contributors to indirect costs were premature death, presenteeism, and absenteeism.
The study used a prevalence-based approach that drew on claims information from the Medicare Current Beneficiary Survey, the Medicare Standard Analytical File and the Optum di-identified Normative Health Information System for direct costs and compared them to direct costs of matched controls without MS.
“DMT costs accounted for 89% of the total outpatient medication expenditure,” the authors noted. “The usage of DMT varied substantially by age group, with about 50% of adults with MS age 18-64 regardless of sex and 21% of men and 40% of women aged ≥65 treated with DMT.” The cost per person of DMT ranged from $57,202 to $92,719, depending on patient age and sex.
While DMTs accounted for the majority of medical costs, limiting their use would likely increase other costs and reduce quality of life. They noted that “studies have shown DMTs to reduce relapses, decrease disability, and improve health-related quality of life. In addition, when patients are treated early, DMTs can delay the progression of disease and reduce the number of new lesions and could lead to lower treatment costs, reduced health care utilization, fewer days of work loss, and lower direct and indirect costs.”
Some indirect costs were calculated from a survey of 946 patients with MS and included productivity losses, cost of paid and unpaid caregivers (who may have given up paid employment), and environmental adaptations. Others, such as premature death, which accounted for 38% of indirect costs, were calculated based on age and the net current value of future earnings. Paid nonmedical care represented 33% of all nonmedical costs, with special equipment or adaptations of home or vehicle driving the 27% of these costs for $202 million. Nontraditional treatments added $342 million to the cost of care.
Disability payments to individuals with MS, about $6.7 billion, were not included in the calculations, as “transfer payments are often used to pay for both medical and nonmedical services, which would double count costs,” the team said.
Looking ahead, the team estimated that by 2039, the U.S. will have approximately 1.2 million people with MS with an associated economic burden of $108.1 billion.
“The findings of this study help underscore the burden of MS in the United States and potential effects of policy or treatment interventions,” the team concluded. “The results suggest a possible role for additional policy initiatives to better support individuals and families affected by MS, in terms of providing treatment and long-term care, worksite support, employment, and occupational training.”
- Bebo B, Cintina I, LaRocca N, Ritter L, Talente B, Hartung D, Ngorsuraches S, Wallin M, Yang G. The Economic Burden of Multiple Sclerosis in the United States: Estimate of Direct and Indirect Costs. Neurology. 2022 May 3;98(18):e1810-e1817. doi: 10.1212/WNL.0000000000200150. Epub 2022 Apr 13. PMID: 35418457; PMCID: PMC9109149.