OMAHA, NB — Even though fewer than 7% of patients with small cell lung cancer (SCLC) survive five years after diagnosis, some patients continue to refuse treatment.
A study team involving researchers from the VA Nebraska-Western Iowa Health Care System and the University of Nebraska Medical Center, both in Omaha, the Medical College of Georgia, Augusta University in Augusta and the University of Indonesia in Jakarta sought to learn more about treatment refusal by patients with SCLC.
The researchers examined factors associated with treatment refusal and the effect of refusal on patient survival.
To do that, they used the National Cancer Database, analyzing data from 107,988 patients with SCLC diagnosed between 2003 and 2012. The study did separate analysis for treatment refusals for chemoradiotherapy among patients with limited stage disease (LS-SCLC) and chemotherapy among those with extensive stage disease (ES-SCLC).
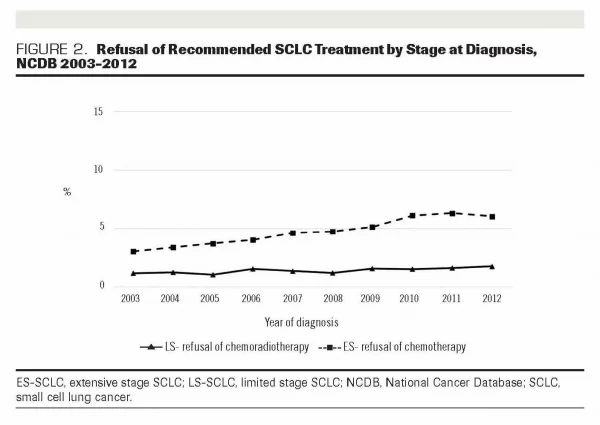
Results indicated that refusal rates of chemoradiotherapy among patients with LS-SCLC and chemotherapy among those with ES-SCLC were 1.34% and 4.70%, respectively.
A concerning finding was that, from 2003 to 2012, trends showed an increase of refusals, especially among the patients with ES-SCLC who were recommended for chemotherapy.
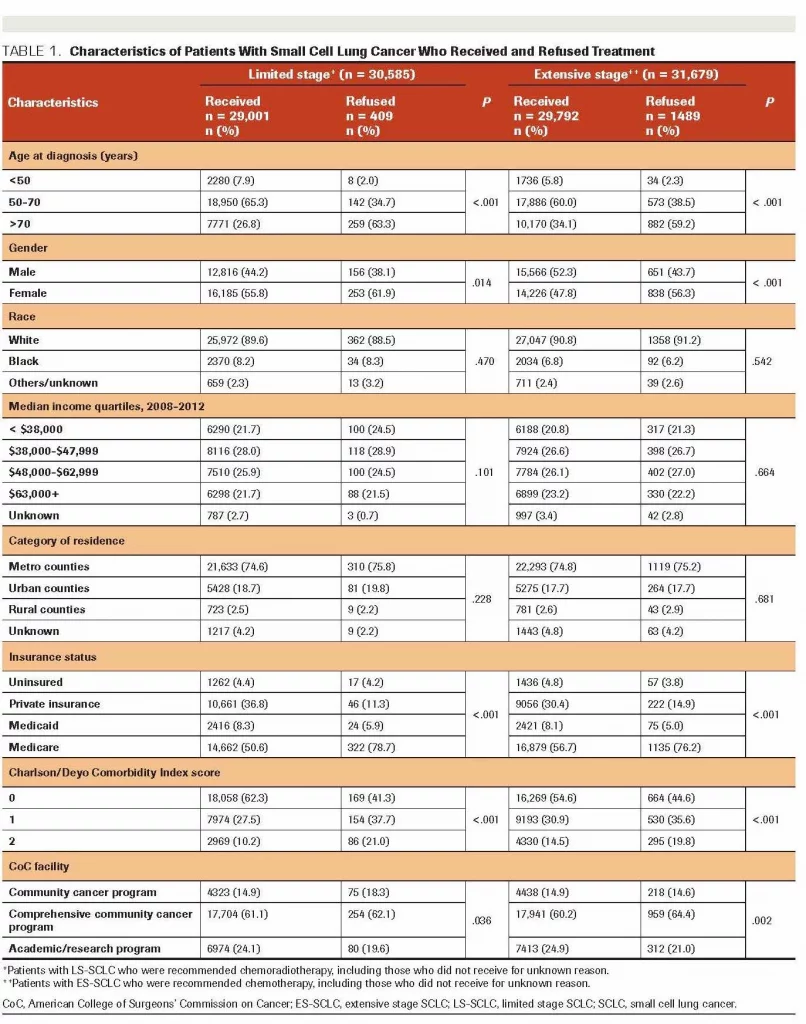
Most associated with treatment refusal in both SCLC groups, according to multivariable analyses, were:
- older age at diagnosis (>70 years),
- female gender,
- uninsured status, and
- presence of comorbidities.
Researchers also determined that patients with LS-SCLC who refused chemoradiotherapy had a substantially higher risk of mortality than those who received treatment (HR, 4.96; 95% CI, 4.45-5.53. The authors reported that the median survival of those who refused treatment was three months, vs. 18 months for those who received it (P <0.001). At the same time, patients with ES-SCLC who refused chemotherapy had a higher risk of mortality than those who received treatment (HR, 3.69; 95% CI, 3.48-3.92); their median survival was one month vs seven months, respectively (P <0.001).
“Treatment refusal among patients with SCLC was associated with worse survival,” the authors concluded. “Strategies to increase patient acceptance of the recommended treatment need to be studied further.”
The issue is not limited to SCLC, according to a new meta-analysis, which found similar issues in non-small cell lung cancer, related to sociodemographic disparities.
The report in the Journal of Thoracic Disease noted that treatment of advanced non-small cell lung cancer (NSCLC) has changed substantially in the past decade with the arrival of biomarker testing, targeted therapies, immunotherapy and palliative care.
“These advancements have led to significant improvements in quality of life and overall survival,” wrote the University of North Carolina at Chapel Hill-led researchers. “Despite these improvements, racial and socioeconomic disparities in lung cancer mortality persist.”
The issue looked at which patients were less likely to receive recommended care.
A narrative overview of the literature was conducted using PubMed and Scopus and was narrowed to articles published from Jan. 1, 2010, until July 22, 2020. The study team looked for articles relevant to sociodemographic variation in (I) chemoradiation for stage III NSCLC, (II) molecular biomarker testing, (III) systemic treatment, including chemotherapy, targeted therapy and immunotherapy, and (IV) palliative and end-of-life care to include in their review.
Ultimately, 22 studies were included. “Sociodemographic disparities in the management of advanced NSCLC varied, but recurring findings emerged. Across most treatment domains, Black patients, the uninsured, and patients with Medicaid were less likely to receive recommended lung cancer care,” they wrote, adding, “Sociodemographic disparities in the management of advanced lung cancer are evident. Given the rapidly evolving treatment paradigm for advanced NSCLC, updated research is needed. Research on interventions to address disparities in advanced NSCLC is also needed.”
- Deviany PE, Ganti AK, Islam KMM. Factors Associated With Treatment Refusal and Impact of Treatment Refusal on Survival of Patients With Small Cell Lung Cancer. Oncology (Williston Park). 2021 Mar 15;35(3):111-118. doi: 10.46883/ONC.2021.3503.0111. PMID: 33818051.
- Stein JN, Rivera MP, Weiner A, Duma N, Henderson L, Mody G, Charlot M. Sociodemographic disparities in the management of advanced lung cancer: a narrative review. J Thorac Dis. 2021 Jun;13(6):3772-3800. doi: 10.21037/jtd-20-3450. PMID: 34277069; PMCID: PMC8264681.