IRVINE, CA—Despite changes in physical training routines and equipment designed to reduce musculoskeletal injuries in servicemembers and veterans, veterans experience back and joint pain at a higher rate than their contemporaries who have never served. For the VA, that translates into an ongoing commitment to explore ways to alleviate pain beyond or in addition to medication. Among the evidence-supported options offered to veterans are acupuncture, mindful exercise such as Tai Chi and yoga, meditation and neuromodulation.
Two-thirds of veterans reported experiencing pain within the last three months in a National Health Interview Survey, with 9.1% classifying the pain as severe. Notably, younger veterans, those under age 40, have twice the rate of severe pain compared to nonveterans their age. Bone and joint injuries are also more likely to be activity-limiting conditions in younger veterans than nonveterans.1
“There’s always this desire to find out more new or novel therapies that can allow us to treat patients from a nonsurgical standpoint to treat pain and provide more function,” David Majors, MD, of the University of California-Irvine School of Medicine, told U.S. Medicine. “At the same time, we don’t want people dependent on opiates.”
As the associate program director for the UC-Irvine residency program, Majors works with residents at the VA medical Center in Long Beach, CA, who were working with neuromodulation to mitigate pain in veterans.
“You might treat acute pain with some of the neuromodulation devices available, but you can’t really do much with chronic pain,” Majors said. “The veterans population is typically a little older population that has to deal with a lot more chronic pain than the average person, so the idea of being able to provide pain relief and also work on the muscles to rehabilitate them really intrigued me.”
Sequential Electrical Stimulation
In an unpublished study, Major and co-author Sujin Lee, of the Rehabilitation Institute, MemorialCare Long Beach Medical Center, Long Beach, CA, analyzed the effectiveness of a device that uses two different waveforms, one to prevent or reverse muscle atrophy and the other to provide deep pain relief. Their study included 1,479 veterans with axial spine, knee or shoulder neuromuscular pain.
For neuromuscular stimulation, the RS-4i plus device uses a low frequency 71 Hz biphasic, asymmetrical waveform that affects both fast-twitch and slow-twitch fibers that prompts a thorough muscle contraction. “The idea is that you can get these muscles to contract and relax, thus allowing for increased circulation, and you can flush some of the metabolites that typically build up in inactive tissue,” Majors explained. “By doing that, you actually activate the muscle, allow the muscle to decrease its risk of disuse atrophy.”
The challenge with muscle stimulation is that the process can be quite uncomfortable, so patients may discontinue use or use it less than would be optimal for rehabilitation.
To overcome this issue, the device also has a pre-modulated, high frequency interferential sine wave delivered at 5,000 Hz across four channels. “That allows you to work not only on acute pain, but also chronic pain,” Majors noted. “It penetrates tissue deeply and really allows for much more thorough pain relief.”
The device couples the two waveforms, alternating between them in sequential electrical stimulation in a treatment called Intersperse. The stimulation can be directly applied to the skin with pads, or the pads can be placed in a vestlike garment that allows flexible placement of up to eight pads on the back.
Study Results
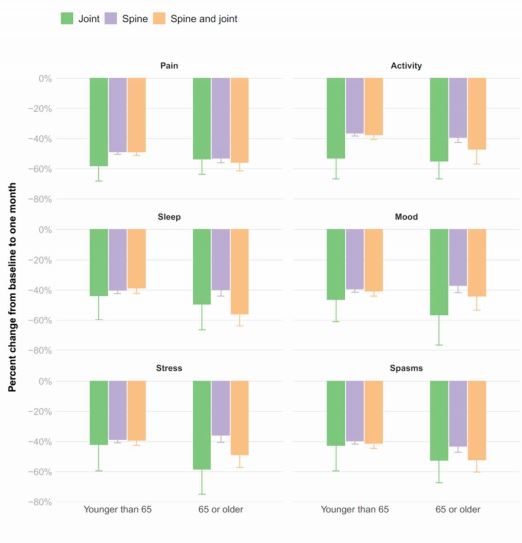
The researchers collected data from veterans at 114 VHA hospitals and outpatient clinics who used the device between 2018 and 2020 to assess the degree of pain relief they received, improvement in function and their satisfaction with the device after one and six months of use. Of the group that had baseline and one-month results, 72.8% were under the age of 65, and 71.8% had used the device for axial pain, 25.7% for combination of joint and spine treatment and 2.4% for joint-only pain.
At one month, all respondents were using the device, and 79% reported using the device at least four time per week, with 77% saying that the device helped them perform daily activities. More than 99% of patients under the age of 65, and 97% of those older than 65 reported that they wanted to continue to use the device, and similar percentages would recommend the device to others.
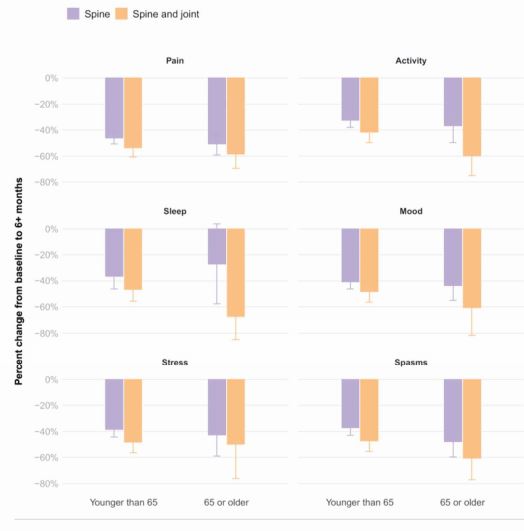
At six months, 96% of participants continued to use the device, and 45% were using it four times a week or more, and 81% said its use helped them perform daily activities. Again, more than 98% wanted to continue use and would recommend it to others. Overall, medication use decreased at one month by 28% and at six months by 31% to 40%, Majors noted.
- Nahin RL. Severe Pain in Veterans: The Effect of Age and Sex, and Comparisons With the General Population. J Pain. 2017 Mar;18(3):247-254. doi: 10.1016/j.jpain.2016.10.021. Epub 2016 Nov 21.