Hospitalized Patients Have RAAS Inhibitors Discontinued, Not Initiated
LOMA LINDA, CA — Inhibition of the renin-angiotensin-aldosterone system (RAAS) plays an important role in reducing morbidity and mortality in patients with heart failure (HF) —one of the most common causes of hospitalization among veterans—particularly in those with HF with reduced ejection fraction (HFrEF).
The benefits of drugs that inhibit RAAS—including angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II type I receptor blockers (ARBs) —have been proven in landmark trials resulting in their incorporation as key elements of guideline-directed medical therapies (GDMTs) for HFrEF. But such trials have been conducted primarily in the outpatient setting and therefore offer little guidance on the drugs’ initiation, continuation or withdrawal in the inpatient setting where there are opportunities for alterations in medication use, explained Roy Mathew, MD, lead author of a new VA study that suggests these drugs are being stopped—or never initiated—in the acute heart failure population.1
Traditionally doctors have been concerned that, when a patient was in an acute decompensated state, using a RAAS inhibitor might worsen heart failure by decreasing cardiac output further decreasing blood pressure, said Mathew, who now is a researcher and nephrologist with Loma Linda VAMC in Loma Linda, CA. Similarly ACE inhibitors and ARBs can lead to lowering of blood pressure, and oftentimes elevations in creatinine, a marker of kidney function and potassium. Mineralocorticoid receptor antagonists, most commonly spironolactone, increase serum potassium, particularly if there is a loss of kidney function, he said.
“Worsened kidney function are hallmarks, or are at least not uncommon, in patients who get acutely decompensated in their heart failure,” Mathew said. “These would be common reasons people would be concerned for either starting or continuing these guideline-directed medical therapies.”
As nephrologists, Mathew and his colleagues were interested in the degree to which changes in kidney function contributed to alterations in guideline-directed medical therapies—and if those changes truly warranted a change in medication that might reduce heart failure morbidity mortality.
Their retrospective study analyzing VHA data of patients hospitalized in 2016 with heart failure with reduced ejection fraction suggested in many cases they weren’t.
The study included 3,652 patients, who were categorized based on the use of ACEI/ARB as continued, initiated, discontinued or no therapy. Of those, 37% of patients hospitalized for AHF had ACEI/ARB discontinued on admission or not initiated.
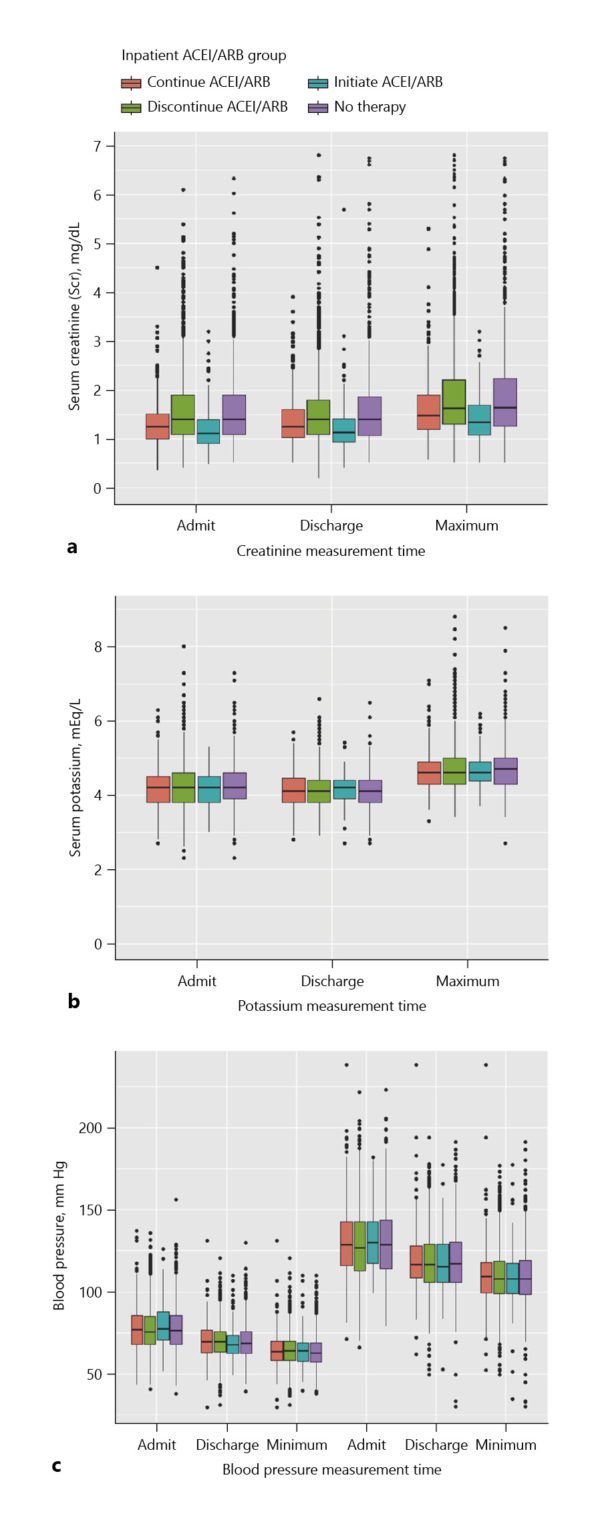
The researchers first looked that participants’ inpatient markers of kidney function—creatinine, systolic or diastolic blood pressure and potassium values. Using 2016 as the index year, they tracked participants through their first hospitalization of the year and looked at the medications that were provided the patient focusing on ACE inhibitors, ARBs, beta blockers, diuretics and mineralocorticoid receptor antagonists—the medication classes that have the greatest evidence of benefit in heart failure population, especially reduced ejection fraction.
Their hypothesis was that that renal function changes were the main driver of the change in medications, so they classified patients in three ways: no change in renal function (compared to their prehospitalization renal function values and inpatient values), worsened renal function on admission and worsened renal function during hospitalization. They then compared that to whether guideline-directed medical therapy was used.
Renal Function
“What we found was that, despite similar blood pressures and serum potassium values across patients who either used or didn’t receive guideline-directed medical therapy, the single most important factor in stopping or not starting therapy was whether or not they had worsening renal function either on admission or during the hospitalization,” said Mathew. A surprising finding, he said, was that the degree of change in renal function was “fairly minimal” for the majority of patients, and there was only a small subset of patients with a truly marked decrease in renal function that would justly cause a concern.
The other surprise, he said, was that, among inpatients who were not started or continued on guideline-directed medical therapy, severe emergency values—markers of potassium greater 5.5 milliequivalents per litre (≥5 mEq/L) or systolic blood pressure less than 90—were actually very infrequent.
“The reason we say that is surprising is that renal function changes by themselves can either be important or not, and we don’t have very good ways of determining other than having ready access to more novel biomarkers which aren’t readily available,” said Mathew. “Unless they are associated with danger markers like very high potassium or very low blood pressure, it is not clear that renal function changes should be determining a lot of the medication changes were see in acute heart failure.”
Although the study focused on veterans, he believes the findings are probably generalizable. “If you compare the rates that we found in discontinuing or not starting guideline-based treatment, it is very similar to non-VA reports.”
Yet, he said he believes such research might not have been possible at non-VA center. “The kind of data that we were able to utilize for our analysis is probably very difficult in a non-VA center, because we were able to use daily changes in both medication and laboratory parameters. I think this a testament to the remarkable health system that the VA is.”
The message of his study for now is awareness, Mathew emphasized, adding, “We are making a lot of decisions on renal function, and it is really not clear that worsening renal function portends a poor outcome always in patients with heart failure,” he said. “We need to examine in more detail, in randomized trials if possible, or at least prospective trials, another way to better evaluate renal function and better utilize guideline-directed medical therapy, regardless of renal function.”
- Mathew RO, Lo KB, Tipparaju P, Phelps E, Sidhu MS, Bangalore S, Herzog C, Vaduganathan M, Tang WHW, Rangaswami J. Patterns of Use and Clinical Outcomes with Angiotensin-Converting Enzyme Inhibitors and Angiotensin Receptor Blockers in Acute Heart Failure and Changes in Kidney Function: An Analysis of the Veterans’ Health Administrative Database. Cardiorenal Med. 2021 Oct 1: 1-11. doi: 10.1159/000519014