FARMINGTON, CT – In many ways, according to a recent study, chronic wounds and pressure ulcers are a geriatric syndrome.
“Older adults are at high risk of developing chronic wounds due to numerous changes that occur with aging. It is reasonable to consider chronic wounds as a geriatric syndrome—highly prevalent, multifactorial, and associated with substantial morbidity and mortality,” wrote University of Connecticut-led researchers.
The researchers pointed out in the Journal of the American Geriatrics Society that the most common chronic wounds diagnosed in older adults are pressure and vascular wounds, including those associated with diabetes.1
Because of the elderly patient population treated by the VA, both in its medical centers and community living centers, the issue of wound care and pressure ulcer prevention has been at the forefront of the healthcare system’s quality improvement efforts.
Three years ago, the VA issued a policy directive, outlining best practices for pressure injury prevention and management and offering advice on technology to manage the dangerous condition. The year before, the U.S. Senate had added pressure-injury prevention as a priority for clinical research, while the U.S. House of Representatives acknowledged that pressure injuries had become a national emergency.
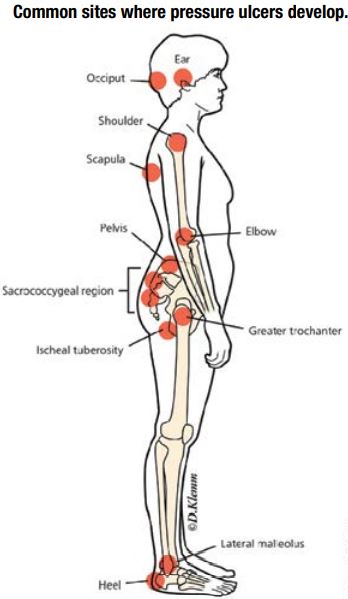 Risk for pressure ulcers increases with well-documented physiologic changes occurring during the aging process. James A. Haley Veterans Hospital and Clinics wrote in a recent study that those include:
Risk for pressure ulcers increases with well-documented physiologic changes occurring during the aging process. James A. Haley Veterans Hospital and Clinics wrote in a recent study that those include:
- decreased body fat,
- decreased muscle mass,
- cellular senescence,
- changes in skin pH,
- decreased metabolism,
- decreased immune function,
- vascular changes,
- altered tissue perfusion,
- nutritional status changes, and
- poor hydration.
“These changes affect skin integrity and wound healing, and raise the risk of pressure-related skin injury,” the study team wrote in Critical Care Nursing Clinics of North America, pointing out that their article “discusses aging as a risk factor for pressure injury (PrI). Topics include evidence for advancing age as a significant PrI risk factor, identifying pathophysiologic changes/mechanisms of aging, and specific PrI preventive interventions to consider in older adults.”
Mayo Clinic researchers put it more bluntly, “The burden of this condition falls largely on older adults, for whom the incidence of chronic wounds far exceeds that of younger populations.”
Their study in Mayo Clinic Proceedings pointed out that Medicare costs for wound care in 2014 were estimated to exceed $28 billion, with prevalence for most wound types highest in patients aged 75 or older.3
Their research also found that venous ulcers are the most common lower extremity wound type, making up 45% to 60% of all wounds, followed by neuropathic ulcers (15% to 25%), ischemic ulcers (10% to 20%), and mixed ulcers (10% to 15%).
Age As Contributing Factor
Major contributing factors, according to another new study, are frailty and the higher likelihood of comorbidities that come with age. University of Utah researchers described how the 5-item modified frailty index (mFI-5) is a validated tool to assess postoperative risks in older surgical patients. In the Journal of Surgical Research, that study team focused on assessing the predictive ability of mFI-5 to its individual components and other established risk factors for complications in flap reconstruction of late-stage pressure ulcer repair.
Results indicated that more than a third, 35.1%, of 1,254 patients receiving flap reconstructive procedures for pressure ulcer repair experienced complications. Most cases had at least one of the following: decreased functional status before surgery, diabetes, history of chronic obstructive pulmonary disease, history of congestive heart failure, and history of hypertension requiring medicine) or other factors commonly used to risk-stratify, such as older age, obesity, ASA classification, and history of smoking.
Much of the VA’s focus has been on nursing homes, where adverse events such as pressure ulcers are leading causes of morbidity and mortality. A study found that how frontline staff typically think about safety and act on safety issues at VA nursing homes or Community Living Centers (CLCs) directly affects rates of adverse events such as pressure ulcer development.
The report in the Journal of the American Medical Directors Association found that better ratings of environmental safety were associated with lower rates of pressure ulcers (OR 0.23, 95% CI 0.09-0.61) as well as other indicators.5
“Nursing homes may reduce adverse events by fostering supportive supervision of frontline staff and a safer physical environment,” reported the team led by the Edith Nourse Rogers Memorial (ENRM) Veterans Hospital in Bedford, MA.
New products also are helping to prevent pressure ulcers in older veterans. A study in the Journal of Wound Care, noted, “Hospital-acquired pressure ulcers (PU) have a substantial negative impact on patients and continue to impose a cost burden on hospital providers. Since the incidence of fragility fracture is growing, driven by the increase in the older population, it is expected that the overall incidence of associated complications will also increase accordingly.”6
Researchers focused on use of a multilayer, silicone-adhesive polyurethane foam dressing for the prevention of PUs in older patients with hip fractures. The measure was cost-effectiveness vs. standard care alone.
The authors determined that the foam dressing intervention was cost-saving and more effective than SP in both Italy and the United States.
“Switching to foam dressing and standard prevention would result in an expected cost saving of €733 per patient in Italy and $840 per patient in the US, reducing the per-patient cost of treating PUs by 37-69% and 36-68%, respectively,” according to the industry-sponsored report.
But, despite the VA’s best efforts, sometimes pressure ulcers are simply not preventable in crisis situations. A recent report in the national Center for Disease Control and Prevention’s Morbidity & Mortality Weekly Report noted that veterans with COVID-19 had more than twice the risk of pressure ulcers than other patients (2.65; 2.14–3.27). 7
- Alam W, Hasson J, Reed M. Clinical approach to chronic wound management in older adults. J Am Geriatr Soc. 2021 May 17. doi: 10.1111/jgs.17177. Epub ahead of print. PMID: 34002364.
- Cowan L, Broderick V, Alderden JG. Pressure Injury Prevention Considerations for Older Adults. Crit Care Nurs Clin North Am. 2020 Dec;32(4):601-609. doi: 10.1016/j.cnc.2020.08.009. PMID: 33129417.
- KP, Kiemele LJ, Stolp AM, Takahashi PY, Verdoorn BP. Prevention, Diagnosis, and Management of Chronic Wounds in Older Adults. Mayo Clin Proc. 2020 Sep;95(9):2021-2034. doi: 10.1016/j.mayocp.2019.10.014. Epub 2020 Apr 8. PMID: 32276784.
- 4. Luo J, Carter GC, Agarwal JP, Kwok AC. The 5-Factor Modified Frailty Index as a Predictor of 30-day Complications in Pressure Ulcer Repair. J Surg Res. 2021 Sep;265:21-26. doi: 10.1016/j.jss.2021.03.011. Epub 2021 Apr 16. PMID: 33872845.
- 5. Quach ED, Kazis LE, Zhao S, Ni P, McDannold SE, Clark VA, Hartmann CW. Safety Climate Associated With Adverse Events in Nursing Homes: A National VA Study. J Am Med Dir Assoc. 2021 Feb;22(2):388-392. doi: 10.1016/j.jamda.2020.05.028. Epub 2020 Jul 19. PMID: 32698990.
- 6. Forni C, Searle R. A multilayer polyurethane foam dressing for pressure ulcer prevention in older hip fracture patients: an economic evaluation. J Wound Care. 2020 Feb 2;29(2):120-127. doi: 10.12968/jowc.2020.29.2.120. PMID: 32058851.
- 7. Cates J, Lucero-Obusan C, Dahl RM, Schirmer P, et. al. Risk for In-Hospital Complications Associated with COVID-19 and Influenza – Veterans Health Administration, United States, October 1, 2018-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020 Oct 23;69(42):1528-1534. doi: 10.15585/mmwr.mm6942e3. PMID: 33090987; PMCID: PMC7583498.

