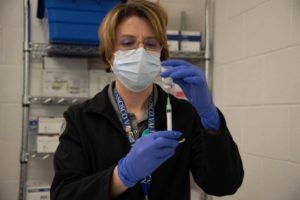
In December 2020, pharmacist Sharya V. Bourdet draws up the first COVID-19 vaccine dose at the San Francisco VAMC. Photo from the San Francisco VAMC’s Facebook page
SAN FRANCISCO — For years, the Institute of Safe Medical Practices and other safety groups have been staunch advocates of technology solutions such as gravimetric verification of drug and diluent volumes and have strongly encouraged their implementation to augment manual processes and provide additional safeguards during sterile compounding.
“Evidence suggests that barcode verification and gravimetrics coupled with real-time alerts created by WFMS can detect and prevent many potentially serious medication errors that would not have been recognized with traditional verification methods,” ISMP pointed out.
VA pharmacies are taking that to heart.
Last fall, members of the pharmacy staff at the San Francisco VA Health Care System presented a webinar on their experience implementing gravimetric intravenous (IV) workflow technology. U.S. Medicine interviewed Sharya Vaughan Bourdet, PharmD, San Francisco’s associate chief of pharmacy, to learn more about the process and lessons learned that could benefit other pharmacy departments in the VA system. The interview has been edited for clarity and brevity.
U.S. Medicine: What prompted you to investigate a new system for IV medication preparation?
Bourdet: This has actually been a journey for us since 2015, when we had different medication errors related to preparing intravenous products. We take patients safety very seriously, so we did a focused review of the process to understand the root causes and identify how we could make changes in the system to prevent those errors from occurring.
What was eye opening in that focused review is that you’re preparing intravenous products, many of which are very high risk chemotherapy hazardous products, and your margin of error is small. You need sterility and accuracy, and it’s heavily reliant on human systems. It made us pause that we have a lot of automation in other areas of the pharmacy, and we didn’t have automation in this very high-risk, high-profile area. It just felt unsatisfying to come up with solutions that were essentially doubling down on the human engineering factors.
U.S. Medicine: What steps did you take to identify a system?
Bourdet: So we did a market analysis that looked at different technology that was available at that time. The barrier for us was the technology interface, our EMR, was not ready yet. VA and federal entities have to lead by example and they have a very high level of security required, so that means there’s a bit of a lag for implementing innovative technology that maybe hasn’t met that security level yet.
U.S. Medicine: How did you get around that issue?
Bourdet: We like to be on the cutting edge, but we’ve learned that building an interface takes an extensive amount of time, effort and testing, which is very valuable for the collective, but the individual facility shoulders a lot of responsibility. At the time, implementing the technology to do what we wanted would have fixed a few things and would have caused other potential errors, so we circled back two years later. By June 2017, the Kansas City VA had started beta testing using the BD IV Prep workflow technology for their oncology infusion center and I was able to visit and see how it could work for us. Then it was a lot of gracious persistence to go through the process of justifying the software and hardware, soliciting bids and securing funding.
U.S. Medicine: When did you actually launch the system?
Bourdet: Our go live was in April of 2020, which was right as COVID hit us. My team thought I was nuts, because I thought we should keep going and not put this on the back burner, because who knew when COVID was truly going to resolve. We worked through it and launched our kick off implementation in April 2020 and full implementation was October 2020.
U.S. Medicine: You’re a year out now. What are the key takeaways?
Bourdet: As with any new technology, folks want to know why, what is this going to do, how is it going to make care better and how is it going to make my job better or worse. We really tied our messaging to safety and highlighted that it made individual jobs better.
For safety, one thing we emphasized was that the system enabled us to take pictures of what is happening in the clean room so the pharmacist can check it remotely and sign off. That’s really important when you have a clean room and the technician is fully gowned and wearing PPE [personal protective equipment]. Previously, the technician would have to stop at certain points and wait for a pharmacist to fully garb, come in, do a visual check and say they’re good to go. That creates a series of interruptions and traffic in and out of the clean room, which is never a good thing, and uses a lot of PPE, which we hadn’t really thought a lot about that [before the pandemic].
Also, there’s much more documentation and timestamping. If there is a question, we can go back and look at what happened, instead of asking people to remember. With increased scrutiny and requirements for documentation through Boards of Pharmacy and the Joint Commission, having documentation within the workflow, rather than having to manually track things down increased efficiencies.
U.S. Medicine: Were you able to quantify increased productivity?
Bourdet: One of our pharmacy residents compared safety and time pre- and post-implementation. Obviously we don’t want any errors to ever reach the patient, but you would like to capture errors before the final check by the pharmacist, because at that final check it’s already been made, and it’s a waste of time and the drug if you have to go back and remake it. IV workflow gives the pharmacist the potential to check at certain time points in the preparation process and send it back and the technician gets an alert saying they pulled up too much and to rework it. (Editor’s note: The gravimetric system links its scale to its visual documentation hardware to ensure the right medication is being prepared at the right dose, which eliminates over- or underfilling because of variability in syringe markings or other devices. It also incorporates hard stops if the weight of the preparation is not within a certain tolerance so the preparer can adjust before moving onto the next step.)
We were definitely able to see increased detection, then after about 90 days, we saw no detection. That’s because people were used to using the system workflow and instead of having over- or under-measurements, they were being accurate themselves and not having to have feedback from the machine. People changed their behavior. The guardrails were still there, but they weren’t hitting them quite as much.
For the time component, we had a couple of factors that impacted time separate from the IV workflow. We had to use our contingency area due to construction during implementation, so we were still able to use the technology for safety and barcode scanning but our staff had to walk across campus to do certain products, so it took more time. We’re doing another follow-up now that we’re back in our original space.
U.S. Medicine: Safety, obviously, is the biggest issue. Did you see any other benefits?
Bourdet: The technology also reduces waste. Previously, if I opened a vial of medication to prepare a bag and didn’t use the whole vial, we would just put it in the fridge and hope people remember that it’s there for the next bag. The software now generates a label in the system with an expiration date and remembers that we have some and it is still good to use, so we’re using our resources better.
U.S. Medicine: What IV products did you include in the system?
Bourdet: We implemented it for all our IV products. We discussed whether to go live with only the hazardous products or chemotherapy and then come back and do the others. Doing it all at once keeps us from having two systems and two different ways of preparing things. I was also concerned that, if there was an error with the nonhazardous IV products, how would we defend that and communicate to a patient or another clinician that we have this technology but we just didn’t use it for that. Doing it for all products is the safer, more equitable option for everybody.
U.S. Medicine: Do you face challenges beyond COVID-19?
Bourdet: With change management, communication is always key. The messaging for us was that we wanted to increase safety for the patient and support the person making it. We had folks that were very engaged and interested in new technology and others that didn’t like using a machine and wanted to do it the way they had for 30 years. We had to address the needs of all those folks and not communicate that we think they’re not accurate or we don’t trust them but that this system can make things better in the following ways.
U.S. Medicine: Do you have any advice for others who are thinking about adopting this system?
Bourdet: Make sure you engage the right team members. Get more people involved and delegate out. There’s a lot of upfront programming needed and you’re essentially building a big library of different drug entries and you have to do all that before implementation. There is a resource library from BD and for other VA sites and we leaned heavily on those that had gone up before us, but there are nuances for each site, in terms of workflow and how you build it that you need to account for.