HOUSTON — More Americans die from heart disease than any other cause, but many fail to take steps known to protect the heart, such as adopting a healthy diet, pursuing regular exercise, and avoiding tobacco use. Even among patients with diagnosed atherosclerotic cardiovascular disease (ASCVD), which includes coronary artery disease, cerebrovascular disease, or peripheral artery disease, relatively few patients follow the recommendations for secondary prevention.
In addition to lifestyle changes, the American College of Cardiology/American Heart Association guidelines recommend pharmacotherapy to reduce low density lipoprotein cholesterol (LDL-C) as well as an antiplatelet along with an anti-hypertensive if needed to control blood pressure for patients with ASCVD. Multiple studies have demonstrated high rates of non-adherence to statin therapy, including among those who have already experienced a cardiovascular event.
Clinicians often note that therapies only work in patients who take them. A previous study in 347,104 veterans with ASCVD provided clear evidence of this maxim, showing a 30% increased risk of death in the least adherent patients compared to the most adherent.1
Younger Patients
While heart disease is often seen as an older person’s illness, the incidence of ASCVD has risen in younger patients since 2000, reflecting the rising rates of three significant risk factors: diabetes, obesity, and hypertension. After a more than 40 year decline, heart disease mortality in patients aged 25 to 64 leveled off starting in 2011 and accounted for nearly 20% of all deaths in this age group in 2017.
A pair of recent VA-led studies provide insight into the challenge of pushing down mortality rates in younger patients.
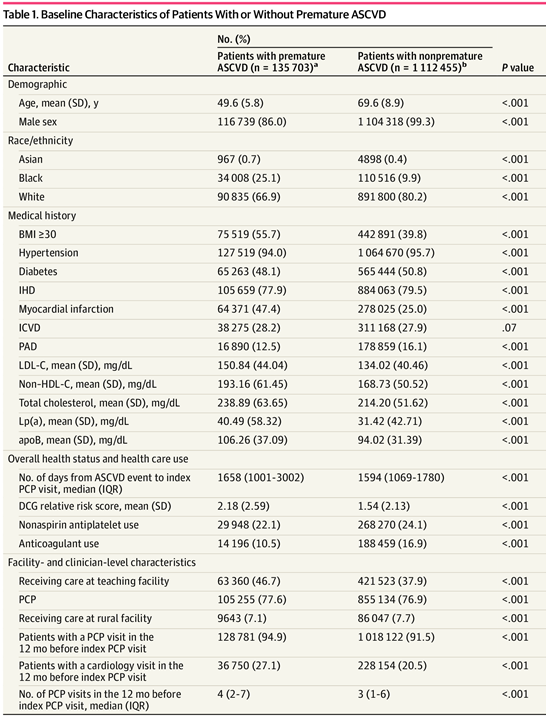
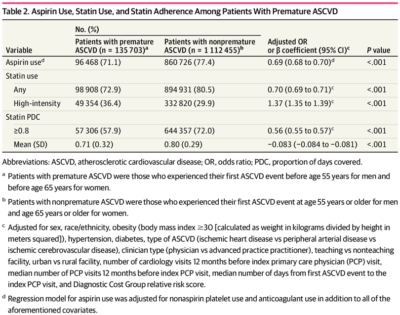
The first found that veterans with premature ASCVD and extremely premature ASCVD were less likely to be prescribed statins or aspirin than veterans diagnosed with the disease at an older age, although all patients had suboptimal use of both medications. Younger patients who were prescribed statins were less likely to continue taking them than older patients. The study defined patients with premature ASCVD as those who experienced their first event earlier than age 55 for men and age 65 for women. First events occurred before a patient turned 40 in those with extremely premature ASCVD.2
The researchers identified several possible reasons for the disparity, including misunderstanding of risk and over-optimism on the part of both clinicians and patients. “Although accurate, the prevailing emphasis on older age as a leading risk factor of ASCVD may create the misperception that younger age has protective properties against ASCVD,” noted Dhruv Mahtta, DO, of the Health Policy, Quality and Informatics Program, Health Services Research and Development, Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VAMC and the Baylor College of Medicine, both in Houston, and his colleagues.
Lower rates of hypertension, diabetes and other metabolic disorders might also cause clinicians to underestimate the seriousness of a younger person’s ASCVD, attribute it to nontraditional risk factors or discount initial ASCVD event as an isolated episode. Clinicians also tend to not increase statin dosage or intensity in patients with extremely premature ASCVD. despite failure to achieve targets, perhaps “because of preconceived notions that these patients do not have as high a risk or do not need high doses at a young age,” the authors said.
Among the young veterans who were prescribed statins, non-adherence rates were high. Lack of understanding of the value of maintaining statin therapy combined with optimism bias boosted by higher functional status after their incident event could contribute to non-adherence. The authors also noted that greater reliance on social media information and less experience with management of chronic conditions may also be factors in lower rates of statin use in younger veterans.
The study included 1,248,158 veterans enrolled in the Veterans With Premature Atherosclerosis (VITAL) registry. Of these, 10.9% had premature ASCVD. The average age of this group was 49.6, 20 years younger than the non-premature group used as a control. Extremely premature ASCVD occurred in 7,716 patients.
Just 71.1% of patients in the premature ASCVD group were prescribed aspirin compared to 77.4% of those with nonpremature ASCVD. Only 72.9% of younger veterans received a statin compared with 80.5% of those in the nonpremature group. Paradoxically, patients with premature ASCVD were more likely to be treated with a high-intensity statin compared with those with nonpremature disease (36.4% vs 29.9%). Just 57.9% of those with premature ASCVD had good adherence to statins, defined as the “proportion of days covered” of at least 0.8, compared with 72.0% of patients with nonpremature ASCVD.
Among veterans with extremely premature ASCVD, less than half were prescribed aspirin (47.5%) or a statin (45.7%) and less than one-quarter (22.7%) were prescribed a high-intensity statin. In this group, only 52% adhered to any statin therapy.
“Future efforts are needed to provide clinician and patient education to discredit misperceptions, conduct qualitative and outcomes research into premature ASCVD, and implement research findings,” the authors said.
That conclusion was well supported by a second study using the VITAL registry and conducted by many of the same researchers from the VA Ann Arbor Health System and Michigan Medicine. That study, published in Cardiovascular Drug Therapy, identified a 50% to 60% variation in the use of antiplatelet agents or any statins in veterans with premature ASCVD between facilities in the VA healthcare system. Statin adherence rates varied by 13% across facilities.3
Marked variation persisted after adjustment for a number of patient-level, facility-level, and provider-level variables, despite class I recommendations for high-intensity statin therapy and at least one antiplatelet agent for every patient with ASCVD and significantly increased morbidity and mortality in the absence of therapies. Veterans with premature ASCVD experienced higher rates of facility-level variability in utilization and adherence to therapies than older patients.
The study included 1,248,158 patients with ASCVD in the VITAL registry. Of the 135,703 veterans with premature ASCVD, 7,716 had extremely premature ASCVD.
“This finding has key implication as a greater degree of variation among young patients with premature ASCVD represents an opportunity to attain a higher lifetime accrued clinical benefit by curbing rates of recurrent adverse cardiovascular events,” the authors wrote. “The extent of facility-level variation observed in our analyses is alarming and calls for improved standardized care and multifaceted interventions to diminish care variation.”
- Rodriguez F, Maron DJ, Knowles JW, Virani SS, Lin S, Heidenreich PA. Association of Statin Adherence With Mortality in Patients With Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2019;4(3):206-213. doi:10.1001/jamacardio.2018.4936
- Mahtta D, Ramsey DJ, Al Rifai M, Nasir K, Samad Z, Aguilar D, Jneid H, Ballantyne CM, Petersen LA, Virani SS. Evaluation of Aspirin and Statin Therapy Use and Adherence in Patients With Premature Atherosclerotic Cardiovascular Disease. JAMA Netw Open. 2020;3(8):e2011051. doi:10.1001/jamanetworkopen.2020.11051
- Mahtta D, Lee MT, Ramsey DJ, Akeroyd JM, Krittanawong C, Khan SU, Sinh P, Alam M, Garratt KN, Schofield RS, Ballantyne CM, Petersen LA, Virani SS. Significant Facility-Level Variation in Utilization of and Adherence with Secondary Prevention Therapies Among Patients with Premature Atherosclerotic Cardiovascular Disease: Insights from the VITAL (Veterans wIth premaTure AtheroscLerosis) Registry7. Cardiovasc Drugs Ther. 2021 Jan 5. doi: 10.1007/s10557-020-07125-3. Epub ahead of print. PMID: 33400053.