Click to Enlarge: Baseline Characteristics of the 200 Sampled Patients With a Diagnostic Code for Long COVID Source: JAMA Network Open
SEATTLE — In the early days and months of the COVID-19 pandemic, the VA and other healthcare systems were focused on the daunting work of helping patients survive the acute effects of the disease. Almost three years later, much of that focus has shifted to helping survivors manage the sometimes lasting after-effects—known as long COVID.
Long COVID was defined in December 2021 by the World Health Organization (WHO) as “the illness that occurs in people who have a history of probable or confirmed SARS-CoV-2 infection; usually within three months from the onset of COVID-19, with symptoms and effects that last for at least two months. The symptoms and effects … cannot be explained by an alternative diagnosis.”
Yet determining whether a patient’s symptoms can be explained by an alternative diagnosis or truly do represent long COVID is one of the challenges clinicians face in caring for these patients, according to a new study highlighting the complexity of diagnosing and managing long COVID in clinical settings.1
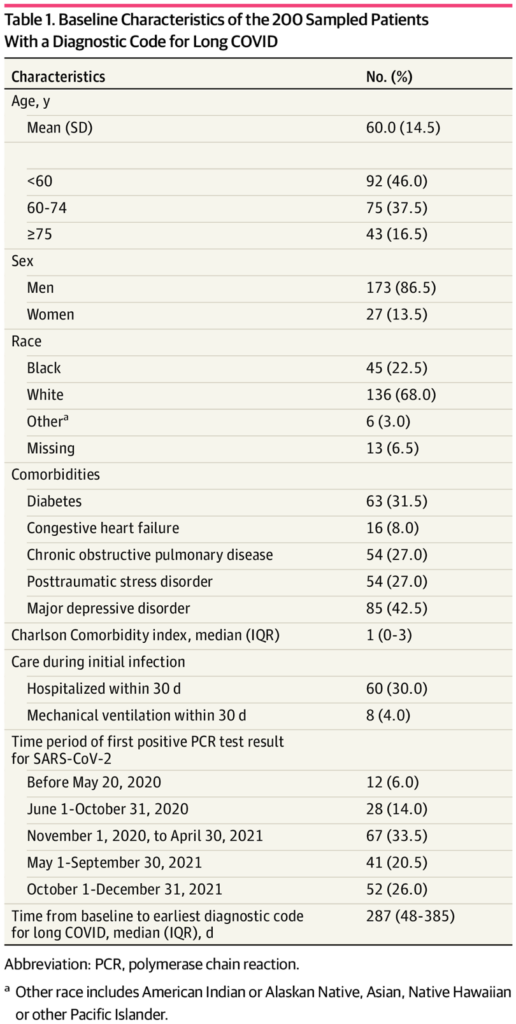
The qualitative analysis used data from the electronic health records (EHR) of a random sample of 200 patients who received care in the VA with a documentation of a positive result on a polymerase chain reaction (PCR) test for SARS-CoV-2 between Feb. 27, 2020, and Dec. 31, 2021, and an ICD-10 diagnostic code for long COVID between Oct. 1, 2021, when the code was implemented, and March 1, 2022. Data were analyzed from Feb. 5 to May 31, 2022.
Using a search tool developed by a member of the research team, which enabled the researchers to locate key data among the overwhelming amount of information in the patient’s medical records, the researchers performed a text word search and qualitative analysis of the patients’ VA-wide EHRs to identify dominant themes pertaining to the clinical diagnosis and management of long COVID.
First Dominant Theme: Clinical Uncertainty
In some cases, the researchers found a diagnosis of long COVID was pretty straightforward. For example, a previously healthy and physically active veteran got COVID-19 and began having symptoms such as fatigue, difficulty with blood pressure or mobility, said Ann O’Hare, MD, a staff nephrologist with the VA Puget Sound Health System in Seattle and the study’s lead author.
“There were some cases like that, but that was unusual,” O’Hare said. “In most cases, it was people who were not physically fit and healthy going into this and had a wide range of other health conditions and a range of symptomatic complaints and functional limitations prior to getting COVID. Then they got COVID, and maybe there was a change in the kind of symptoms they were having or the intensity or the character of symptoms, but it was pretty subtle,” she said.
“It just became very difficult for the clinicians and veterans themselves to distinguish what was really COVID and what wasn’t. That, I would say, was one of the biggest findings.”
This lack of certainty often meant that people with suspected long COVID were referred for further testing and evaluation, which led to the second major theme the study uncovered—care fragmentation.
Second Dominant Theme: Care Fragmentation Post COVID
“When patients were referred to long COVID clinics or post-COVID clinics—they had a variety of different names—often they would get a comprehensive evaluation from a multidisciplinary team consisting of psychologists, physical therapists, occupational therapists and clinicians, but that care would really be siloed from the rest of the care that they were getting,” O’Hare said. Further, primary care clinic notes tended to list prior SARS-CoV-2 infection as a discrete item in the clinical assessment and plan, disconnected from patients’ other problems and presenting concerns, the study found.
Rethinking the Management of Long COVID
“I do think it is important for us to think carefully about how we define long COVID and understand the complexity of patients in the real-world setting, because I do worry that having a long list of possible symptoms can make it really hard to identify the problem and lead to more testing and more care as clinicians try to figure out long COVID,” O’Hare said.
The key message of the study is the importance of ensuring the care of veterans who develop complications of COVID-19 are integrated with the rest of their care, so they are not receiving duplicate care or more care than they need, O’Hare said. “I think there is a need for better integration with existing care process and to really focus on a veteran-centered approach where you are really focusing on what these veterans need and what we can do to help them rather than what does the person have,” O’Hare said.
“It’s just difficult to know—it’s hard to determine if what they are experiencing is just an exacerbation of their underlying comorbid conditions or a true consequence of the virus,” she said. “In many cases, it may not be possible to know, and maybe it doesn’t matter too much if you can provide them with what they need.”
- O’Hare AM, Vig EK, Iwashyna TJ, Fox A, et. al. VA COVID Observational Research Collaboratory (CORC). Complexity and Challenges of the Clinical Diagnosis and Management of Long COVID. JAMA Netw Open. 2022 Nov 1;5(11):e2240332. doi: 10.1001/jamanetworkopen.2022.40332. PMID: 36326761; PMCID: PMC9634500.
