Relationship of VA organizations.Source: OIG analysis of organizational charts located in Department of Veterans Affairs 2020 Functional Organization Manual Version 6
SPOKANE, WA — The initial rollout of VA’s new electronic health record (EHR) system at the Mann-Grandstaff VAMC was deeply flawed and requires serious reconfiguring.
That’s according to a recent report from the VA Inspector General’s Office, as well as the department’s own investigation. While VA leaders are still standing by the CERNER-developed system, they admitted that the VA staff at Spokane was not adequately trained and that CERNER’s technical support fell short of VA’s needs.
VA Secretary Denis McDonough appeared before the Senate VA Committee last month to talk about the department’s findings and what VA plans to do next. Many of the legislators—some of whom have been dealing with VA’s EHR issues for more than a decade—exhibited significant frustration and not a little exhaustion at this latest roadblock in VA’s $16 billion project.
“Nearly nine months ago, VA rolled out its new electronic health record at the Mann-Grandstaff VA Medical Center,” said committee Chair Sen. Jon Tester (D-MT) in his opening statement. “At the time, VA officials described the rollout as ‘flawless.’ The former secretary said it was revolutionary and boasted that ‘we just pulled off the most expensive IT program in government history.’ He said he only heard ‘crickets’ from the critics because it had gone so well. Well, guess what? Since a lot of those statements were made, we’re hearing from VA medical staff who are frustrated and demoralized by a new system that is making their jobs more difficult. … So while some might describe this as a ‘flawless’ rollout, I think most people would use words like ‘alarming’ or something far worse.”
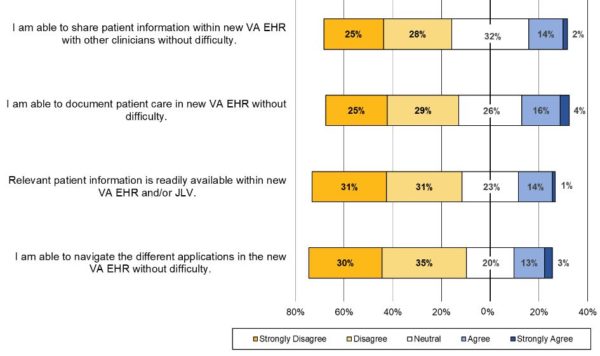
Click to Enlarge: Facility staff responses to an OIG survey on EHR use.
Source: OIG analysis of the survey results
The IG report concurred with Tester’s assessment, noting that the rollout plan neglected to comprehensively train staff to use the system as a whole.
“Facility leaders reported that training did not provide opportunities to test proficiency in navigating a wide variety of clinical scenarios; instead, instruction focused on the multiple steps required to complete specific tasks. Facility leaders coined the term ‘button-ology,’” the report states. “One facility staff training coordinator reported, ‘It was just people sitting down and learning to use buttons and not having any context for what they were doing.”
OIG investigators discovered significant gaps in training staff for clinical workflow and that Spokane staff had been left with an incomplete understanding of how to apply what little training they received to their daily tasks.
VA paused the rollout in April to conduct a 12-week assessment of the launch at Spokane after hearing many of the same complaints that the IG reported.
“I heard from [one clinician] that help with the new platform wasn’t always easy to find, even when you asked for it,” McDonough told the committee. “When she called the CERNER help desk, the person on the other end of the line told her he’d just started a week prior. She had more experiencing using the platform than the person who was supposed to help her navigate it. Stories like that were what led me to launch the top-to-bottom review.”
VA’s review also found that the people who were going to use the system—VA clinical staff—had been left out of the planning process for the rollout.
‘Run in a Silo’
“The project was run in a silo,” McDonough said, “which means that some relevant stakeholders did not have a chance to shape its success. In fact, the IG report … found no evidence that our healthcare experts in VHA had a defined role in decision-making or oversight. [There was a] distinct lack of testing and training for a real-life clinical environment.”
The findings fall well short of a catastrophe, however, McDonough declared. “Most challenges were not due to breakdowns in technology or the people at Mann-Grandstaff. The missteps were ours at VA and CERNER. Now that we’ve identified those problems, we can solve them.”
That solution involves a complete restructuring of the rollout going forward. The plan had been for VA to move on to implement the system at facilities in the Midwest then return to the Pacific Northwest. Prior to that, VA had expected to roll its system out parallel with the Military Health System’s (MHS) GENESIS, also built by CERNER. As the MHS rollout pulled far ahead of VA, that parallel rollout was scrapped.
Now, McDonough said, VA will have to create a new roadmap for rolling out their EHR—one that can adapt and shift as the project moves forward.
“First we’re establishing a unified enterprise wide governance effort led by our deputy secretary,” McDonough explained. “This structure will incorporate key clinical, technical, acquisition and finance leaders, guaranteeing that everyone who will build this platform will use it or be affected by it and work in concert from Day One.”
Secondly, VA will shift from a concrete roadmap to one based on a readiness approach.
“We’re going to deploy the program based on evidence of readiness,” McDonough said. “Which sites are most trained and technologically ready for it. Thereby setting each new site up for success. [We’ll] create a simulated testing and training environment so veterans and providers can properly learn and evaluate the system before it goes live, not during or after.”
Where the system will rollout to next is a decision that McDonough says he might not make until the end of 2021, noting that VA has questions it needs answered about patient safety and access.
“I think we can get our hands around that by this fall, but I won’t go live at [the Midwest and Pacific Northwest] sites until we’ve answered those questions fully,” McDonough declared.
Legislators also had questions about the choice of going with a CERNER-created EHR in the first place. CERNER was initially chosen because the company was also the manufacturer of GENESIS, and the long-term goal of both MHS and VA systems is interoperability and the seamless sharing of patient records.
That goal has not yet been achieved, McDonough conceded. While patient data from VA, DoD and community care providers are all individually available to VA clinicians, they “do not all populate the same screen at the same time, which is kind of the point.”
“One doc told me ‘the only place where it’s all aggregated is in the clinician’s head,’” McDonough added. “We’ve got to get to the place where that’s not the case.”
That response had legislators wondering whether the CERNER system was worth fixing or whether VA should cut its losses. And, if problems persist, would there be a way to hold CERNER accountable?
“Through this review I’ve satisfied myself,” McDonough said. “I think the technology is basically sound. Much of the technology questions in terms of execution end up being [about] governance.”
