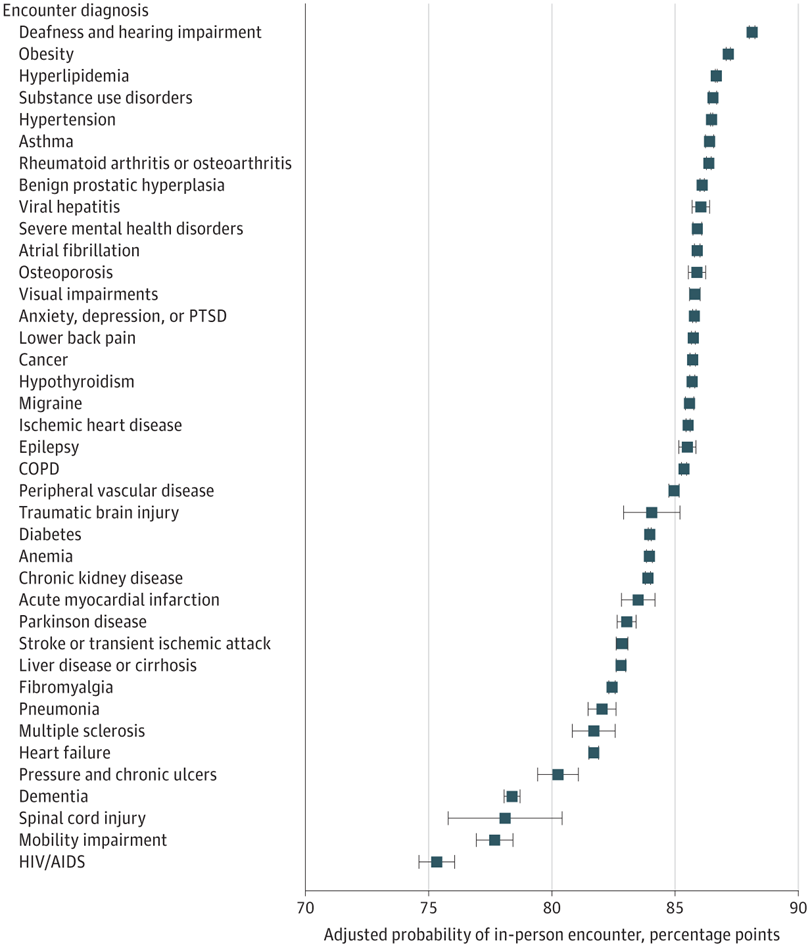
Click To Enlarge: Model was adjusted age, gender, race, ethnicity, rurality, marital status, VHA enrollment priority group, drive time from a primary care facility, facility complexity, and other chronic conditions managed during the encounter. Results are derived from a Poisson regression modeling the likelihood of an encounter occurring in-person when a chronic condition is coded in the encounter diagnoses vs not coded. Estimated margins are reported to illustrate the probability of an encounter occurring in-person.
PALO ALTO, CA — As telehealth continues to evolve from a pandemic-era necessity to a core component of modern care, a new national study of VA outpatient encounters revealed that the likelihood of a visit being conducted in person, by phone or via video might hinge on the patient’s chronic condition.
The analysis, which examined more than 7 million VA primary care visits between April 2022 and March 2023, found that, while 83.2% of encounters still took place in person, 11.1% occurred by telephone and 5.8% by video. Yet this distribution was far from uniform across health conditions.1
“Since the COVID-19 pandemic, the VA has rapidly expanded its offerings of telehealth,” said Jacqueline Ferguson, PhD, a health services researcher at the VA Palo Alto Center for Innovation to Implementation. “We know that telehealth use tends to be higher among younger veterans, women veterans and Veterans living in urban areas. It also depends on whether clinics and patients have the right equipment and internet access and whether the patient believes video visits are a good way to receive healthcare. But what is not well understood is which specific health conditions—like high blood pressure, back pain or heart failure—are being treated using telehealth.”
That is what prompted the study, which was published in JAMA Network Open, she said.1
Using diagnosis codes from VA electronic health records, Ferguson and her team categorized each primary care visit by mode of delivery and by the condition addressed. They identified 39 chronic conditions and analyzed how frequently each was associated with in-person, phone or video visits. Importantly, the study used only de-identified administrative data, preserving veterans’ privacy.
Conditions requiring physical exams or lab tests—such as chronic obstructive pulmonary disease (COPD), ischemic heart disease and anemia—were more likely to occur in person. Conversely, conditions related to mobility challenges or where physical assessment was less essential—like dementia and Parkinson’s disease—were more often managed through video.
“These findings suggest that the clinical conditions being addressed during an encounter may be associated with the probability of a health care encounter being in person or via telephone or video,” the authors wrote.
Ferguson said the extent of variation in visit modality came as a surprise. “The variation in whether a visit with different chronic conditions occurred by phone or video compared to in-person was more pronounced than we expected,” she said. “For example, visits with a deafness or hearing impairment diagnosis had a 4.5% probability of being video-based, but visits with a dementia diagnosis had a 10.7% probability of being video-based.”
The findings suggested that video visits might play a valuable role for conditions that impair travel or benefit from visual observation. Video use was highest for conditions like dementia (10.7%), HIV/AIDS (8.8%), pressure ulcers (8.0%) and Parkinson’s disease (7.5%).
“For veterans with dementia or Parkinson’s, video visits may be easier than an in-person visit,” Ferguson explained. “Dementia can make it hard to navigate to unfamiliar places, and Parkinson’s can make physically leaving the house more difficult. Video care also offers a convenience factor for caregivers, who can easily join the appointment and be active participants in veterans’ healthcare.”
The study authors noted that “video-based care provided some value for conditions where visual assessment can provide value in the management of that clinical condition,” such as Parkinson’s disease and traumatic brain injury. These visits may allow clinicians to observe gait, facial expression or tremors, even when an in-person exam isn’t feasible.
Despite its benefits, telehealth was not the dominant mode for most chronic conditions. Only three—heart failure, HIV/AIDS and mobility impairment—were more likely to be managed via telehealth than in person. Ferguson attributes this in part to the need for physical assessments, labs and imaging.
“Many of these conditions appeared to be those in which a physical examination is often required … or when laboratory or diagnostic evaluations guide therapy,” the study authors wrote.
The findings underscore that, while telehealth can increase access, it also has limitations—and these must be carefully considered when designing care models. “Ensuring that veterans are receiving the right type of care at the right time is critically important,” Ferguson told US Medicine. “Relying entirely on telehealth isn’t ideal, as providers might miss something that an in-person exam would have caught. But having every visit in-person can also be a barrier, making it harder to have regular check-ins and potentially allowing chronic conditions to worsen or go untreated.”
The solution, she suggested, may lie in hybrid care models tailored to each patient. “The key is to find the right balance that meets both clinical and practical needs,” she said. “We suspect that a hybrid care model that blends in-person and telehealth visits based on the patient’s conditions, needs and desire for telehealth is the right approach.”
As healthcare systems continue to use and develop more robust telehealth infrastructure, “these findings may be helpful in building models, pathways, and guidelines for such programs and clinical care,” the authors wrote. “Few clinical guidelines provide guidance about when to offer telehealth or in-person care,” the study authors noted. “Looking at how often telehealth is used for specific conditions could be a valuable guide.”
Ultimately, Ferguson said, data-driven insights like those from this study are essential to ensure equitable and effective care delivery. “As clinicians and policymakers work to find the right balance between telehealth and in-person care, looking at how often telehealth is used for specific conditions could be a valuable guide,” she said.
- Ferguson JM, Greene L, Van Campen J, Zulman DM, Wray CM. Variability in Primary Care Telehealth Delivery Methods Across Chronic Conditions. JAMA Netw Open. 2025 Mar 3;8(3):e251988. doi: 10.1001/jamanetworkopen.2025.1988. PMID: 40136302; PMCID: PMC11947845.

