ALBEQUERQUE, NM — As every military strategist knows, winning a battle depends on knowing your adversary’s vulnerabilities. In the last decade, that same approach has transformed cancer therapy.
At the VA, the National Precision Oncology Initiative leads the effort to characterize each veteran’s cancer through genomic analysis and use that information to target its weaknesses. Within that program, the Lung Precision Oncology Program (LPOP) aims to increase lung cancer screening in high-risk veterans, expand genomic testing, and increase access to precision oncology trials for those diagnosed with lung cancer. The program is a collaboration between the VA’s Office of Research and Development, National Oncology Program Office and Office of Healthcare Transformation.
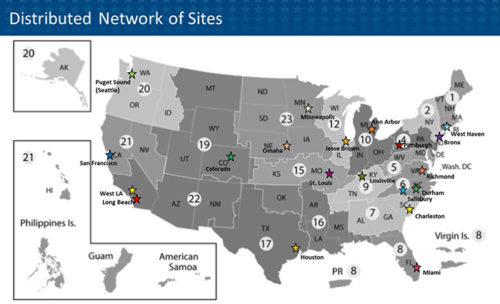
LPOP includes 20 “hub” locations around the country which coordinate care and research, as well as more than 100 locations that administer chemotherapy. As of May 2021, more than 5,000 veterans had completed molecular testing for their lung cancers.
The program aims to improve care of veterans with lung cancer by offering genetic testing for those with advanced disease, improving access for those veterans to precision oncology clinical trials, expanding the number of clinical trials available to veterans, and bring new treatment options to veterans through clinical trials. As an integrated treatment and research program, LPOP’s goals also include “enabling rapid translation of discoveries into clinical care” and creating a “learning healthcare system for administrative, clinical care and research purposes,” according to the VA.
Explosion in Targeted Agents
Precision oncology is fundamentally different from classic cancer treatment, which administers the same few therapies or used the same procedures for all patients at the same stage of a cancer. Precision medicine matches patients with specific molecular characteristics—germline or inherited genetic variations, mutations in their tumors or even features of the gut microbiome—to a therapeutic agent that targets that variant. Correlating treatment with patient-specific characteristics reduces toxicities, increases the likelihood of response, improves survival outcomes, and reduces costs and wasted time associated with fruitless treatment.
In non-small cell lung cancer (NSCLC), precision medicine has focused on addressing metastatic disease because of its grim prognosis and its rapidly expanding, but highly targeted, armamentarium. The U.S. Food and Drug Administration (FDA) announced approvals for 15 drugs or combinations to treat NSCLC in the last 18 months. All were for patients with tumors that expressed (or did not express) specific mutations, and all but one were for use in the advanced or metastatic setting.
Since the start of 2021, FDA approvals for therapies to treat advanced or metastatic NSCLC included:
- Tepotinib for patients harboring mesenchymal-epithelial transition (MET) exon 14 skipping alterations;
- Cemiplimab-rwlc for patients whose tumors have high PD-L1 expression with no epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK) or c-ros oncogene 1 (ROS1) aberrations;
- Lorlatinib for patients with tumors that are ALK-positive;
- Sotorasib for patients with KRAS G12C mutated tumors who have received at least one prior systemic therapy; and
- Mobocertinib for patients with EGFR exon 20 insertion mutations, whose disease has progressed on or after platinum-based chemotherapy.
The rapid approval of agents to treat advanced and metastatic disease has driven seven revisions to the National Comprehensive Cancer Network (NCCN) guidelines so far this year. Because of the highly specific nature of the systemic therapies used to treat metastatic NSCLC, the NCCN guidelines recommend molecular testing for all patients with Stage 4 disease. Further, the guidelines panel “strongly advises broader molecular profiling with the goal of identifying rare driver mutations for which effective drugs may already be available, or to appropriately counsel patients regarding the availability of clinical trials. Broad molecular profiling is a key component of the improvement of care of patients with NSCLC.”
From Testing to Treatment
Conducting next-generation sequencing (NGS) multigene panels for broad molecular profiling is only part of the battle of bring precision medicine to every veteran with advanced or metastatic NSCLC, however. The benefit to the patient comes from using the results of the testing to guide treatment decisions, and their researchers have found a disconnect in VA care.
A team led by Vishal Vashistha, MD, of the Raymond G. Murphy, New Mexico VAMC discovered that “a substantial minority of patients with NSCLC bearing highly actionable gene variants are not prescribed targeted agents.”1
Of the 1,749 veterans with advanced NSCLC who received NGS gene panel testing between July 2015 and February 2019, 112 or 5.4% had Level 1 or 2A evidence for available targeted treatments. Almost one-third of those patients (32.1%) were not prescribed a targeted agent, even though the “highly actionable gene variants were within ALK, BRAF, EGFR, ERBB2, MET, RET, and ROS1” which have multiple available targeted therapies.
The researchers found that physicians failed to prescribe the appropriate therapy for three main reasons. One-third said they did not prescribe a targeted therapy because the patient did not have metastatic disease, although most of the targeted agents are also approved for advanced NSCLC. A quarter of the physicians made no comment and took no action on the NGS results. Just under one in five doctors thought the patient would not tolerate the therapy.
The team recommended “further provider- and pathologist-directed educational efforts and implementation of health informatics systems to provide real-time decision support for test ordering and interpretation.”
- Vashistha V, Armstrong J, Winski D, Poonnen PJ, Hintze B, Price M, Snowdon JL, Weeraratne D, Brotman D, Jackson GP, Kelley MJ. Barriers to Prescribing Targeted Therapies for Patients With NSCLC With Highly Actionable Gene Variants in the Veterans Affairs National Precision Oncology Program. JCO Oncol Pract. 2021 Jul;17(7):e1012-e1020. doi: 10.1200/OP.20.00703. Epub 2021 Mar 29. PMID: 33780286.