In most recurrent prostate cancer patients, androgen-deprivation therapy works for a while. Eventually, however, most men end up developing castration-resistant prostate cancer. Now, expanding treatment options are especially benefitting older men in that situation, who often didn’t fare well with chemotherapy.
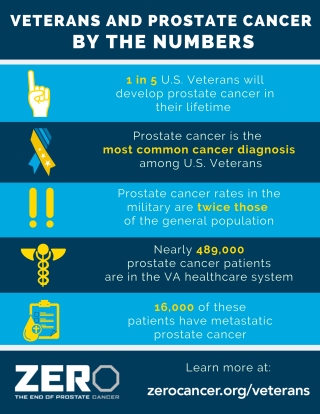
PORTLAND, OR — Every year, about 15,000 veterans develop prostate cancer, with the risk of the disease rising sharply with age. For the 20% to 30% of veterans who will experience a recurrence of the cancer following initial surgery or radiation, the options for treatment have been fairly limited because of concerns about comorbidities, frailty and inability to tolerate chemotherapy.
The first-line treatment for recurrent prostate cancer is androgen-deprivation therapy (ADT), which induces medical castration. More than 90% of recurrent or metastatic cancer patients respond to ADT initially, but, in time, nearly all men on the therapy will develop castration-resistant prostate cancer (CRPC).
Fortunately, the options available for veterans with CRPC have dramatically expanded in recent years, and recent studies show that these options are effective and suitable even for men in their 80s.
“The older population has a higher risk of prostate cancer morbidity and mortality and has unique issues around drug tolerability, metabolism, and polypharmacy,” noted Julie Graff, of the VA Portland Health Care System, and her colleague at the Oregon Health & Science University in Portland, Zizhen Feng. “The rise of nonchemotherapy treatment options for prostate cancer gives men more treatment options, particularly for those patients who are not suitable for chemotherapy.”1
Three second-generation androgen receptor inhibitors are indicated for nonmetastatic CRPC (nmCRPC) in conjunction with continued ADT—apalutamide, darolutamide and enzalutamide. Apalutamide and enzalutamide are also approved for use in men with metastatic CRPC (mCRPC), as is abiraterone. “The majority (86%) of men with mCRPC initially had nmCRPC that became metastatic rather than initially presenting with metastatic disease,” Graff and Feng wrote. “Delaying the time to metastasis is critically important.”
A pooled analysis of clinical trials of second-generation androgen receptor inhibitors performed by investigators in the FDA’s Office of New Drugs and published in Lancet Oncology found that, in patients with nonmetastatic CRPC who had a prostate-specific antigen doubling time of less than 10 months and were 80 years of age or older, the estimated median metastasis-free survival was 40 months in the androgen receptor inhibitor arms and 22 months in the placebo arms, for an adjusted risk reduction of 63%. Those results compared well with the median metastasis-free survival seen in younger men of 41 months in the androgen receptor inhibitor groups and 16 months in the placebo groups, for an adjusted reduction in metastasis risk of 69%.2
The median overall survival in patients aged 80 and older was 54 months in the intervention groups compared to 49 months in the placebo groups, for a 21% reduction in mortality risk. That compared to 74 months in the next-generation androgen receptor groups and 61 months for the placebo groups in men younger than age 80.
Advantages and Challenges
While the recent approvals provide a welcome alternative to often difficult-to-tolerate chemotherapy and also offer benefits in terms of progression-free and overall survival, they should be used with a full understanding of their risks, interactions and contraindications. Graff and Feng drilled down into the base studies to identify the advantages and potential challenges in older men of the three next-generation hormonal therapies approved by the U.S. Food and Drug Administration for treatment of nmCRPC.
The SPARTAN trial compared apalutamide to placebo. In men aged 75 and older, the drug increased metastasis-free survival 59% and progression-free survival 41%. Grade 3 or 4 adverse events were common in both the intervention and placebo arms in this age group, 50.4% and 37.4%, respectively. The risk of falls was 18.9% in the apalutamide group and 13.4% in the placebo group. Additional follow-up to the SPARTAN study showed median overall survival benefit of 22%, though data for the oldest group was broken out.
The PROSPER trial evaluated metastasis-free survival for enzalutamide compared to placebo. Overall, the next-generation androgen inhibitor reduced the risk of metastasis 71% compared to placebo, 36.6 months vs. 14.7 months. Median overall survival was 67 months with enzalutamide and 56.3 months with placebo. For men age 75 and older, the use of the drug reduced mortality risk 19%. As with previous trials, three patients in PROSPER who received enzalutamide experienced seizures. Men in the treatment group also had higher risk of fatigue, hypertension and falls across all age groups than men who received placebo.
The ARAMIS trial looked darolutamide versus placebo. Among men aged 75 to 84 years, darolutamide reduced the risk of metastasis 57% compared with placebo. For those 85 and older, risk of metastasis declined 49%. Overall risk of death declined 31% with darolutamide, but specifics by age group were not available. Patients with seizure were not excluded from the ARAMIS trial because of the low penetration of the blood-brain barrier by the drug, and 0.2% of patients in both arms experienced seizures. Darolutamide was not associated with higher risk of falls, fractures, fatigue, cognitive impairment or hypertension than placebo in the broad patient population, though safety information on those age 75 and older was not available.
The researchers concluded that “these three drugs shared similar and significant efficacy, with [metastasis-free survival] improvements of approximately two years over placebo and [overall survival] improvement, both of which remained significant in the subgroup” age 75 and older. They encouraged clinicians to consider the difference in adverse events, drug-drug interactions, as well as drug availability when selecting a treatment for older men with nonmetastatic CRPC.
- Feng Z, Graff JN. Next-Generation Androgen Receptor-Signaling Inhibitors for Prostate Cancer: Considerations for Older Patients. Drugs Aging. 2021 Feb;38(2):111-123. doi: 10.1007/s40266-020-00809-3. Epub 2021 Feb 9. PMID: 33559101.
- Fallah J, Zhang L, Amatya A, Gong Y, et. al. Survival outcomes in older men with non-metastatic castration-resistant prostate cancer treated with androgen receptor inhibitors: a US Food and Drug Administration pooled analysis of patient-level data from three randomized trials. Lancet Oncol. 2021 Sep;22(9):1230-1239. doi: 10.1016/S1470-2045(21)00334-X. Epub 2021 Jul 23. PMID: 34310904.