A review of renal cell carcinoma surveillance in a four-state region found that veterans treated at the VA had a significant incidence of high-risk lesions and poor compliance with follow-up imaging. The answer, according to the authors, might be much more aggressive biopsy protocols to make sure treatment is optimal, especially with so many patients lost to follow-up. Unlike in the past, patients diagnosed with advanced RCC have many more options for long-term remission.
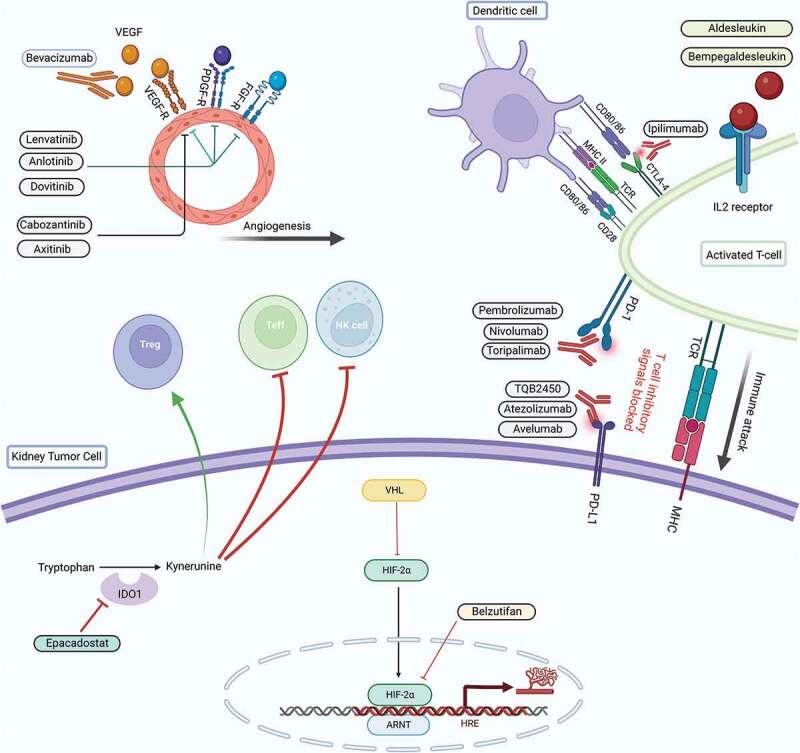
Click to Enlarge: Mechanism of action of the newer drugs currently being investigated in advanced RCC.32. Source: Human Vaccines & Immunotherapy
AURORA, CO — Discerning whether a small renal mass poses a risk to a patient can be challenging. Imaging often provides little assistance in distinguishing benign from malignant masses, limiting the options for noninvasive determination.
Consequently, the American Urologic Association’s current guidelines recommend biopsy for any lesion with unclear pathology and when a determination will affect clinical decisions. Results from a biopsy can help patients and clinicians evaluate the appropriate options, including active surveillance (AS), nephrectomy (partial or radical) or cryoablation.
Renal mass biopsy (RMB) may be more important at the VA than in other care environments, as veterans have an elevated risk of renal cell carcinoma, a disease that has become increasingly prevalent in the U.S. In 1999, the U.S. Centers for Disease Control and Prevention reported 33,020 cases of kidney and renal pelvic cancers. Over the next 20 years, the number of cases in the U.S. more than doubled, exceeding 68,000 by 2019. During the same period, the incidence rate rose from 12.2 to 17.2 per 100,000. The National Cancer Institute’s Surveillance, Epidemiology, and End Results Program projects that there will be 82,800 cases of kidney and renal pelvis cancer in 2023 and nearly 15,000 deaths.
Renal cell carcinoma (RCC) accounts for approximately 90% of all renal cancers. Veterans have a higher risk of RCC than the general population for a variety of reasons, including that veterans tend to be older and male, and the average age for diagnosis of RCC is 64. Veterans also are more likely to be or have been smokers, be obese and have hypertension or diabetes—all risk factors for RCC, which occurs twice as often in men than in women. In addition, active-duty servicemembers are more likely to be exposed to chlorinated solvents, petrochemicals and heavy metals, all of which confer a grater RCC risk.
Researchers at the Rocky Mountain Regional VAMC in Aurora, CO, and the University of Colorado Anschutz School of Medicine, had a hunch that RCC was being undertreated in the four-state VA healthcare system, so they undertook a quality improvement study that reviewed results of renal mass biopsies and analyzed follow-up and compliance over a 5-year period.1
The team identified 136 renal mass biopsies in veterans in the region between June 2015 and November 2020. Based on the findings, they categorized eight as non-diagnostic (group 0), 40 as benign masses/minimal risk (group 1) and 76 malignancies as of average aggressiveness (group 2). Group 3 included 12 unexpectedly aggressive lesions, such as papillary type 2 RCC, grade 4 or sarcomatoid clear cell RCC (ccRCC) or unsuspected urothelial cell carcinoma.
Group 1 masses were considered suitable for active surveillance. Group 2 included grade 1-3 ccRCC, papillary type 1 RCC and chromophobe RCC, where the findings did not change the management plan developed based on imaging. Group 3 biopsies “significantly altered the standard treatment plan and led to consideration of radical nephrectomy, wide local resection or other aggressive treatment,” the researchers said.
For patients with the high-risk cancers in group 3, treatment beyond surgery may be needed. That could include radiation or other therapies. For urothelial cell carcinoma, chemotherapy may be recommended, but neither chemo nor monotherapy with targeted therapies have shown benefit in sarcomatoid or papillary RCC. For these aggressive forms of RCC and advanced RCC, patients are likely to require the use of checkpoint inhibitors combined with VEGFR-tyrosine kinase inhibitors (TKI) and may later need a multiple receptor TKI combined with an immune checkpoint inhibitor.
Small Masses Surprisingly Risky
The Rocky Mountain team drilled down into the data to see whether biopsies of smaller masses, specifically, provided valuable clinical information. Among the masses of 4 cm or less size that were completely within the kidney (T1a), the VA team found that the results of the biopsy changed the management plan in 40 out of 101 cases. Twelve of the others in this group were excluded from later analysis, either because of non-diagnostic results from biopsy or determination that they were decompressed cysts.
Among the masses of 4 cm or less size that were completely within the kidney (T1a), the team found that the results of the biopsy changed the management plan in 40 out of 101 cases. Twelve of the others in this group were excluded from later analysis, either because of non-diagnostic results from biopsy or determination that they were decompressed cysts.
Of the remaining 89 patients, 12 had benign findings that did not require follow-up. Among the 77 with solid masses eligible for follow-up analysis, 56 received cryoablation or underwent surgery and 21 chose active surveillance. Half of those who elected active surveillance (AS) had oncocytoma or RCC based on their biopsies.
Most notably, the team found that 9% of these smaller masses were unexpectedly aggressive variants, which differed from previous studies that have shown a more indolent course and no difference in overall mortality between active surveillance and primary intervention.
The authors noted that, “while AS is an effective management strategy, it is highly dependent on patient compliance with follow-up appointments and imaging, as well as the assumption that small renal masses are generally biologically indolent,” which the surprisingly high rate of aggressive lesions calls into question in the VA population.
In addition, the researchers found that the compliance rate in this study was only 60% and trended downward over time, even with implementation of regular reminders by email and phone calls of the timing and need for appointments. “Despite these efforts, follow-up imaging compliance was concerningly low at all-time points. This is consistent with other research showing poor follow-up appointment adherence in the veteran population,” they said. “Therefore, active surveillance may confer unrecognized risks in our patient population.”
The Takeaway
“In the VA population and underserved populations with limited access to healthcare, or who have higher rates of housing insecurity, toxic exposures, smoking/alcohol use, etc., I would say more patients should be treated rather than be on active surveillance,” co-author Kseniya Anishchenko, MD, who is now with the University of Pittsburgh Department of Medicine, told U.S. Medicine. “In our VA cohort, patients had transportation issues or mistrust of the medical system that I think caused follow-up visits to be low.”
The study reinforced how important it is for “clinicians [to know] their population and keep societal factors in mind when making treatment plans—such as looking at the no-show rates of their patients,” Anishchenko added. “It is important to aggressively treat if you think there are a lot of barriers to a patient getting healthcare.”
Based on the study results, “every mass less than 4 cm should be biopsied,” she said. “In our VA cohort, we found a higher incidence of highly aggressive small masses than expected; knowing this about the VA population means we should biopsy small masses whenever possible.”
One reason that is so important is that greatly improved treatments for advanced RCC are rapidly coming online.
“Currently, treatment of advanced or metastatic renal cell carcinoma involves targeting the most relevant molecular pathways implicated in cancer initiation and progression,” said researchers from the Huntsman Cancer Institute in Salt Lake City. “Results of the ongoing Phase III trials are expected to provide important breakthroughs. In addition, there still exists an unmet need for the predictive biomarkers to guide the best initial choice of therapy and to optimize the sequential use of available therapeutic agents. The future holds a strong possibility to witness more immune combinations that hopefully will allow us to achieve long-term remission, and even cure more patients with metastatic RCC.”
The report in Human Vaccines and Immunotherapeutics said those trials include the CLEAR Study, among others. CLEAR was a three-arm trial involving 1,069 participants and investigated pembrolizumab/Lenvatinib, everolimus/Lenvatinib, or sunitinib in treatment-naïve patients. The results led to the Food and Drug Administration approval of pembrolizumab/lenvatinib for first-line treatment of adult patients with advanced RCC.2
- Anishchenko K, Antoine S, Geiger C, Lenzmeier R, Kim S, Lloyd GL. High-risk Disease and Poor Follow-up: The Importance of Renal Mass Biopsy in a Cohort of Veterans. Urology. 2022 Sep;167:152-157. doi: 10.1016/j.urology.2022.05.006. Epub 2022 May 16.
- Gebrael G, Sahu KK, Agarwal N, Maughan BL. Update on combined immunotherapy for the treatment of advanced renal cell carcinoma. Hum Vaccin Immunother. 2023 Dec 31;19(1):2193528. doi: 10.1080/21645515.2023.2193528. Epub 2023 Apr 16. PMID: 37062953; PMCID: PMC10114990.
