Veterans have higher rates of cirrhosis, hepatitis C infection, obesity, high alcohol use and diabetes—all of which put them at greater risk of hepatocellular carcinoma. Treatment is challenging, and a new study found that it tends to be inconsistent across regions within VA healthcare, with the West providing more interventions and having longer survival.
WASHINGTON, D.C. — Veterans are five times as likely to have hepatocellular carcinoma, the most common type of liver cancer, compared to the general population, and a recent study has found differences in treatment patterns and overall survival rates across the VA’s five geographic regions.
In 2021, a total of 2,000 veterans in VA care were diagnosed with hepatocellular carcinoma, according to a VA spokesperson.
“VA enrollees have a higher incidence of hepatocellular carcinoma (HCC) because they have higher rates of most of the important risk factors for HCC,” a VA spokesperson told U.S. Medicine. “For example, compared to the general population, VA enrollees have higher rates of cirrhosis, hepatitis C infection, obesity and diabetes. Another factor is the risk of alcohol use is higher in veterans, in part related to trauma.”
“Finally, metabolic risk factors for nonalcoholic fatty liver disease are higher in veterans than civilian populations due to Agent Orange exposure. Other factors that are associated with increased risk of HCC are being male and older, both of which are higher among the veteran population in comparison to the general population.”Treatment of hepatocellular carcinoma is challenging, the VA spokesperson explained in an email. There are multiple treatment options, and choosing the appropriate treatment for each patient is time-consuming and complicated. Most patients with hepatocellular carcinoma can receive palliative, locoregional or potentially curable treatment. However, hepatocellular carcinoma recurs in the majority of veterans within two to three years of treatment.
The retrospective study published in the journal Annals of Surgical Oncology used the VA Corporate Data Warehouse to build a comprehensive national dataset of veteran patients with hepatocellular carcinoma diagnosed between 2001 and 2015 to compare patients across VAHS regions.1
The study analyzed 13,434 patients and found the West region had the highest rate of overall treatment receipt (63.6%), and the Southwest had the lowest rate (52.9%). After adjusting for demographic, clinicopathologic, treatment and hospital factors, treatment in a non-West region continued to be significantly associated with a 10% to 13% increased risk of five-year mortality, according to the study.
The researchers concluded that treatment patterns and overall survival rates of hepatocellular carcinoma patients differ significantly across VAHS geographic regions. They suggested that targeted interventions to increase the rate of treatment in the non-West regions are needed to improve survival of veterans with hepatocellular carcinoma and provide uniformly high-quality care across VAHS facilities.
“VA is committed to providing veterans the soonest and best care,” the VA spokesperson wrote in an email. “We carefully review variations in care between VA medical centers and across regions and are involved in a continuous process of closing gaps as the evidence emerges.”
Investigating improved techniques for diagnosing liver cancer is a high research priority, the VA spokesperson explained in an email. This year, the VA has launched one of the largest liver cancer screening research studies in its history. The focus of the work is whether an abbreviated magnetic resonance imaging (aMRI) is more effective at detecting hepatocellular carcinoma in early stages than ultrasound, the current standard of care.
The study is scheduled to recruit 4,700 veterans with cirrhosis from 47 VAMCs. Cirrhosis is a known risk factor for liver cancer.
“By increasing early detection, our medical researchers believe VA will be able to increase successful outcomes,” the VA spokesperson added.
According to a review article published in Gastroenterology Research, hepatocellular carcinoma is the fastest-rising cause of cancer mortality in the United States. It is the fourth-most-common cause of cancer-related mortality worldwide, and incidence increased by 75% worldwide between 1990 and 2015, with 800,000 annual deaths. Data from the Global Burden of Disease Study reported that liver cancer deaths increased by 25% from 2010 to 2019.2
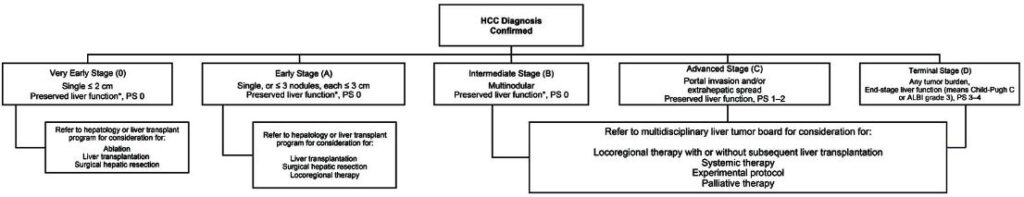
Click to Enlarge: HCC staging algorithm [54]. HCC: hepatocellular carcinoma; ALBI: albumin-bilirubin; PS: ECOG performance status. Source: Gastroenterology Research
The review article supports the importance of early detection of hepatocellular carcinoma. The article found that early detection of hepatocellular carcinoma improves options for potentially curative treatment, which is associated with significantly improved five-year survival.
Patients diagnosed with advanced stages of hepatocellular carcinoma survive a median of one year and up to two years with systemic therapy. Effective implementation of hepatocellular carcinoma screening and surveillance in patients with cirrhosis is associated with improved early-stage diagnosis of hepatocellular carcinoma, while suboptimal hepatocellular carcinoma surveillance has led to a high proportion of hepatocellular carcinoma being detected at advanced stages, according to the article.
The review article provides a summary of the existing gaps in hepatocellular carcinoma care by reviewing data on surveillance rates, disparities associated with hepatocellular carcinoma surveillance and targeted efforts to improve hepatocellular carcinoma surveillance. It also introduces a free, open-access decision-support tool that has been developed to assist healthcare professionals in the surveillance, diagnosis, staging and treatment of patients with hepatocellular carcinoma.
The tool incorporates guideline-based recommendations on hepatocellular carcinoma surveillance and staging systems and could improve appropriate and timely triage of patients to appropriate care. This tool was developed by the Hepatocellular Carcinoma Steering Committee of the Chronic Liver Disease Foundation and is targeted toward clinicians across specialties who may encounter liver lesions during routine care or as part of dedicated hepatocellular carcinoma surveillance.
- Ju MR, Karalis JD, Chansard M, Augustine MM, Mortensen E, Wang SC, Porembka MR, Zeh HJ 3rd, Yopp AC, Polanco PM. Variation of Hepatocellular Carcinoma Treatment Patterns and Survival Across Geographic Regions in a Veteran Population. Ann Surg Oncol. 2022 Dec;29(13):8413-8420. doi: 10.1245/s10434-022-12390-7. Epub 2022 Aug 26. PMID: 36018517.
- Wong RJ, Jayasekera C, Jones P, Kanwal F, Singal AG, Ahmed A, Taglienti R, Younossi Z, Kulik L, Mehta N. An Open-Access, Interactive Decision-Support Tool to Facilitate Guideline-Driven Care for Hepatocellular Carcinoma. Gastroenterology Res. 2022 Dec;15(6):297-307. doi: 10.14740/gr1573. Epub 2022 Dec 1. PMID: 36660470; PMCID: PMC9822660.
