Active-duty servicemembers who have mental health disorders need continued support when they are deployed, according to a new study that underscored the need for in-theater healthcare providers. The Uniformed Service University of the Health Sciences-led authors also found that women were more likely to report mental health issues, including serious types, such as bipolar disorder.
BETHESDA, MD — Mental health is a significant concern within the U.S. military, and deployed servicemembers regularly undergo demanding and stressful experiences that can contribute to mental health challenges.
About 20% of the active duty population was diagnosed with at least one mental health disorder in 2016. However, there are few studies examining rates of mental health disorders in-theater, which refers to an area in which important military events occur or are progressing.
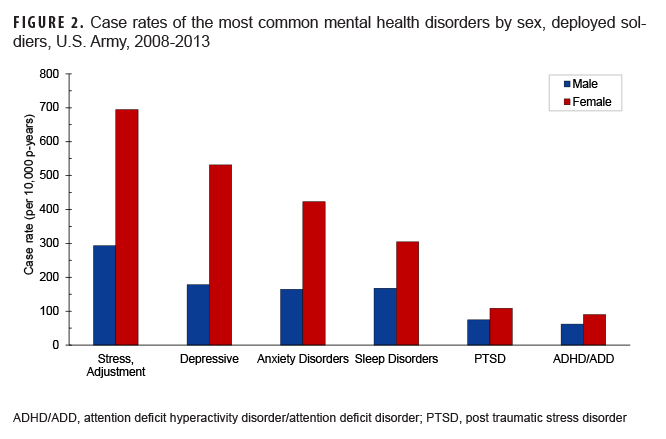
A Uniformed Services University of the Health Sciences-led study of mental health disorders among deployed U.S. Army soldiers found the highest case rates included stress reactions and adjustment disorders, depression, anxiety and sleep disorders, and female soldiers had consistently higher rates than their male counterparts.
The report, “In-Theater Mental Health Disorders Among U.S. Soldiers Deployed Between 2008 and 2013,” part of a Medical Surveillance Monthly Report, a peer-reviewed journal of the Armed Forces Health Surveillance Division. The most significant finding of the in-theater mental health study was that rates of diagnosis of mental health disorders in the U.S. military population differ by sex.1
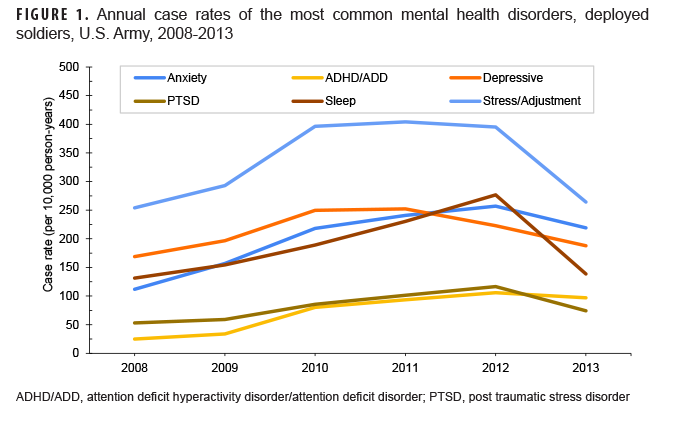
In this report, case rates were calculated across 12 categories of mental health disorders using diagnostic encounter data from the Theater Medical Data Store. The study cohort consisted of 530,404 active duty servicemembers in the U.S. Army who were deployed to an overseas contingency operations area between the calendar years 2008 and 2013.
The disorders with the highest case rates in-theater included stress reactions/adjustment disorders, depression, anxiety and sleep disorders, followed by post-traumatic stress disorder (PTSD) and attention-deficit disorder (ADD)/attention-deficit/hyperactivity disorder (ADHD). The lowest rates among deployed soldiers were for psychosis, bipolar, somatic and eating disorders.
The results highlighted the crucial need for in-theater behavioral health providers to effectively deliver short-term treatments for stress, anxiety, depression and sleep disruptions. The findings may also contribute to developing new policies and interventions to better prepare, support and treat soldiers during deployments, according to the report.
A recent VA study pointed out that, even though conditions like bipolar disorder are less common, history of trauma correlates with worsening outcomes in those patients. The study in Psychiatric Research looked at associations between trauma exposure (type and timing) and suicide attempt in veterans with bipolar disorder.1
Researchers from the Durham, NC, VAMC, Duke University and colleagues had 106 veterans with a diagnosis of bipolar disorder and 815 veterans with no psychiatric history (age rage = 20-72 years old) complete a clinical questionnaire, the Beck Scale for Suicide Ideation, and the Traumatic Live Events Questionnaire.
The researchers analyzed the data for correlations with diagnosis, time of trauma (before, during, or after the military), trauma type (attack, illness, accident, child violence, child sexual abuse and adult sexual abuse) and suicide attempt.
Results indicated that 75 veterans with bipolar disorder had comorbid PTSD. “Controlling for PTSD, veterans with bipolar disorder had a higher prevalence of trauma including physical assault [odds ratio (OR) = 2.85; 95% confidence interval (CI) = 1.39-5.86] and child sexual trauma (OR = 2.89; CI = 1.38-6.05),” the authors wrote. “Veterans with bipolar disorder who endorsed previous suicide attempts (n = 42) had significantly higher levels of exposure to childhood trauma (OR = 5.69; CI = 1.84-17.62).”
The researchers suggested that a history of previous trauma exposure should be taken into account when assessing veterans at risk for bipolar disorder, especially trauma characterized as attack and childhood sexual abuse. “Particular attention should be given to Veterans with bipolar disorder and exposure to trauma during childhood, which may be associated with increased risk of suicidality,” they added.
Higher Rates of Diagnosis
Female soldiers had higher rates of serious mental illness such as bipolar disorder than their male counterparts, but the actual numbers were low, according to the authors. Women make up more than 17% of military personnel.
“Across all of the disorders we examined, female soldiers had consistently higher rates of diagnosis than their male counterparts,” said co-author David Riggs, PhD, director of the Center for Deployment Psychology at the Uniformed Services University of the Health Sciences in Bethesda, MD, told U.S. Medicine. “To our knowledge, this is the first study of mental health diagnoses among deployed troops that has shown this. Notably, the rates of disorders reported in our study are not limited to newly diagnosed disorders, they include cases that were receiving treatment for an existing diagnosis.”
The data show that many servicemembers are receiving care for mental health disorders, even while deployed.
“If a servicemember is experiencing a mental health concern, whether at home or in-theater, they should know they are not alone and that seeking help does not mean that they will face adverse consequences,” Riggs wrote in an email. “By acknowledging this, maybe we can help to reduce the stigma associated with seeking care. We have many effective evidence-based treatments that can help.”
Riggs suggested that healthcare providers of all types must evaluate patients for mental health symptoms and treat or refer as appropriate. However, healthcare professionals cannot make these diagnoses or referrals unless they see the patients.
“We also need military leaders to help encourage service members to talk about and seek care for mental health concerns,” Riggs wrote in an email. “This may include things like changing the way they talk about mental health or correcting misperceptions about receiving a diagnosis.”
Providers and leaders also should also keep in mind that many mental health conditions are not necessarily permanent conditions, and they are often exacerbated by high levels of stress, such as those that occur during combat deployments. Servicemembers should be reevaluated after deployments to determine if the condition remains once the stress of the deployment is alleviated. If the condition no longer exists, healthcare providers should see that the medical record reflects that the condition or disorder has resolved, Riggs explained.
These results are notable because they are different from what is expected for some disorders that are generally more prevalent among males than females. For example, previous studies suggest males should have higher rates of alcohol and/or substance-use disorders or attention deficit hyperactivity disorder than females.
“Our data are also somewhat different from studies of service members and veterans who have returned from combat that suggest only small sex differences in the psychological impact of combat deployments,” Riggs wrote. “It is important to keep in mind that our results were based on diagnoses made in the medical records, so we were not able to look at what may have led to this difference in rates.”
There are several possible explanations for the sex differences found in the study.
“First, it is possible, though unlikely, that deployed females do experience all of these mental health disorders at greater rates than deployed males,” Riggs explained. “Other factors seem likely to have influenced the rates we observed and are important to consider. To receive a diagnosis in the medical record, a soldier must have sought care from a healthcare provider. Thus, willingness to seek care and experience of stigma likely influenced the observed rates. It is possible that female soldiers are more likely than male soldiers to seek care from professionals. We have data from another study that suggests that female soldiers experience less cohesive connection with the soldiers in their unit than do male soldiers, which may lead them to seek support elsewhere, like from healthcare professionals.”
“We must also consider the possibility that healthcare providers are more likely to diagnose female soldiers than male soldiers with a mental health disorder when the soldiers do seek care. We do not know that this is occurring, but such a bias could also contribute to the findings of this paper. More research is needed to confirm the difference that we observed and to help us understand the factors that contribute to these differences,” Riggs added.
- Paxton Willing MM, Tate LL, O’Gallagher KG, Evatt DP, Riggs DS. In-Theater Mental Health Disorders Among U.S. Soldiers Deployed Between 2008 and 2013. MSMR. 2022 Nov 1;29(11):11-17. PMID: 36790903.
- Fijtman A, Clausen A, Kauer-Sant’Anna M; VA Mid-Atlantic MIRECC Workgroup. Electronic address: [email protected]; Morey R. Trauma history in veterans with bipolar disorder and its impact on suicidality. J Psychiatr Res. 2023 Jan;157:119-126. doi: 10.1016/j.jpsychires.2022.10.063. Epub 2022 Nov 2. PMID: 36463626.