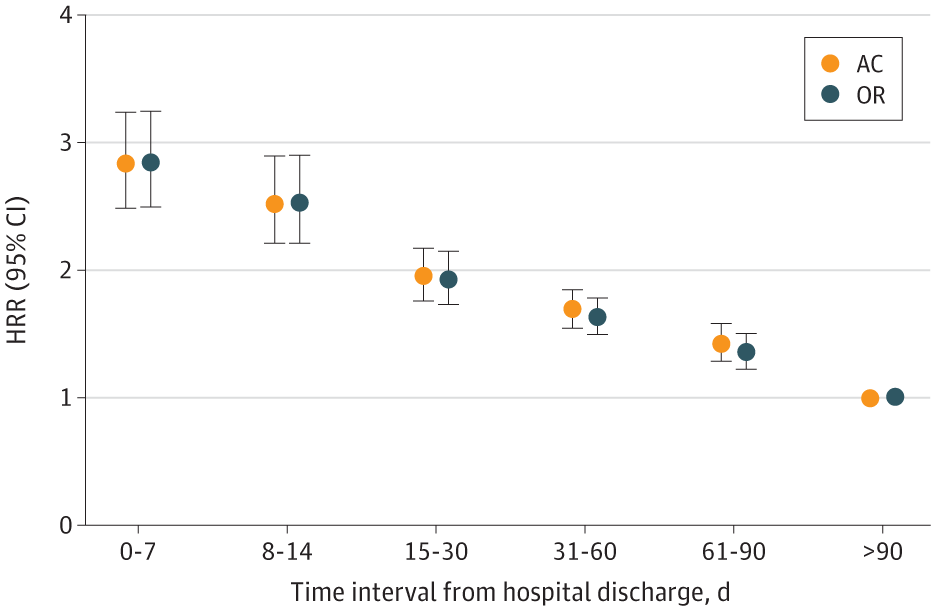
Click to Enlarge: Risk of Opioid-Related (OR) and All-Cause (AC) Mortality Within Different Time Intervals After Hospital Discharge Among Veterans With Opioid Use Disorder Hazard rate ratios (HRRs) are presented for each time interval after discharge from an index medical hospitalization compared with a reference interval of 91-365 days. Source: JAMA Network
SALT LAKE CITY, UT — Past research has revealed that patients who are hospitalized for substance-use disorders appear to have an elevated risk of death, but little information was available on when and why.
A new veteran’s study sought to answer those questions.
A study team led by the University of Utah and the Salt Lake City, UT. VA Healthcare found that the risk of death after a medical hospitalization was highest the first week after discharge and incrementally decreased over a one-year observation period.
Their report in JAMA Internal Medicine also pointed out that few patients were prescribed naloxone or buprenorphine around the time of hospitalization.
“These findings highlight the need for intensive support for patients with OUD in the immediate posthospitalization period,” the authors wrote. “Emerging care models such as inpatient addiction consult teams may improve care transitions and mitigate elevated overdose risk after hospitalization.”
The study noted that about 1 in 9 hospitalized patients in the United States has a substance-use disorder SUD, explaining, “The high prevalence of SUD among hospitalized patients makes hospitals especially important venues for identifying patients with SUD and offering real-time access to treatment. However, medical hospitalizations also represent periods of destabilization.”
The authors advised that the “sequelae of acute medical illness, SUD-related vulnerability, and unfavorable contextual and environmental factors may synergize, increasing risk of overdose, readmission, and death immediately after hospital discharge.”
In fact, that is exactly what has been reported by some regional studies, but those were short on specifics, according to the article.
For the study, researchers used a national VHA sample to estimate the risk of opioid-related and all-cause mortality during prespecified time periods after hospital discharge among patients with OUD. The goal was to gain better understanding of when patients experience the highest risk of harm after hospital discharge so that tailored interventions and targeted patient support can be developed.
VHA records were linked to the Mortality Data Repository to determine mortality and cause of death during a 1-year observation period after an index hospitalization (defined as first medical hospitalization in the study period). Adjusting for sex, race and ethnicity, and age, the model compared the interval risk of opioid-related and all-cause mortality within 0-7, 8-14, 15-30, 31-60 and 61 to 90 days, compared with 91 to 365 days, after discharge.
The authors pointed out that data on race and ethnicity were based on self-reports and included as potential factors in study outcomes. The study team also controlled for comorbid health conditions in assessing all-cause mortality.
The study included 98,890 veterans with OUD who experienced 1 or more medical hospitalizations during the study period; they had a median age of 59 and were 93% male.
Within the 1-year observation period, 7,683 deaths occurred (7.8%), and 848 of those (11%) were determined to be opioid-related.
In the total sample, only 5.2% were prescribed naloxone within about 30 days of index hospitalization, and only 6.5% were prescribed buprenorphine during the hospitalization and/or within 30 days of discharge, according to the researchers.
They calculated rates of opioid-related death per 1000 person-years as:
- 13.4 (95% CI, −4.0 to 30.9) for 0-7 days,
- 14.4 (95% CI, −3.0 to 31.8) for 8-14 days,
- 9.8 (95% CI, −0.7 to 20.2) for 15-30 days,
- 9.0 (95% CI, 1.9-16.2) for 31-60 days,
- 10.8 (95% CI, 4.1-17.4) for 61-90 days, and
- 8.6 (95% CI, 6.5-10.7) for 91-365 days after a medical hospitalization.
“Compared with the window of 91 to 365 days, risk of dying from opioid-related causes in the first 7 days after hospitalization increased nearly 3-fold (hazard rate ratio [HRR], 2.85; 95% CI, 2.5-3.3; P < .001),” the authors noted. “Results were similar for all-cause mortality (HRR, 2.80; 95% CI, 2.5-3.2; P < .001).”
The study team advised that limitations included the reliance on administrative records to determine OUD diagnosis, patient characteristics and key outcomes, as well as the use of VHA data alone.
“Further investment in care models that facilitate addiction treatment initiation in the hospital followed by rapid linkage to care is needed to improve safety for patients with OUD,” the authors concluded.
- Incze MA, Huebler S, Baylis JD, et al. Mortality Among Veterans With Opioid Use Disorder After Medical Hospitalization. JAMA Intern Med. Published online April 07, 2025. doi:10.1001/jamainternmed.2025.0356

