Click to Enlarge: Note: VA’s medically underserved initiative assists underserved facilities in the adoption of strategies and identification of available resources to improve access to care at medical facilities where veteran requests for care exceed the facility’s ability to meet those needs in a timely manner
WASHINGTON, DC — For the past several years, VA has been identifying the most underserved facilities in its system and requiring them to create action plans to improve care to their veterans. A recent report from the Government Accountability Office (GAO) has found, however, that the effort has achieved little and might have a negative impact on hiring and a demoralizing effect on current staff.
According to VA, approximately 16% of veterans live in areas with a shortage of primary care services, and 70% live in areas with a shortage of mental healthcare services. Part of the MISSION Act requires the department to “inform and assist” facilities that were most unable to meet the demands for care.
In 2019, VA began identifying the 10 most underserved facilities in its system—the top five most underserved for primary care and the top five most underserved for mental healthcare.
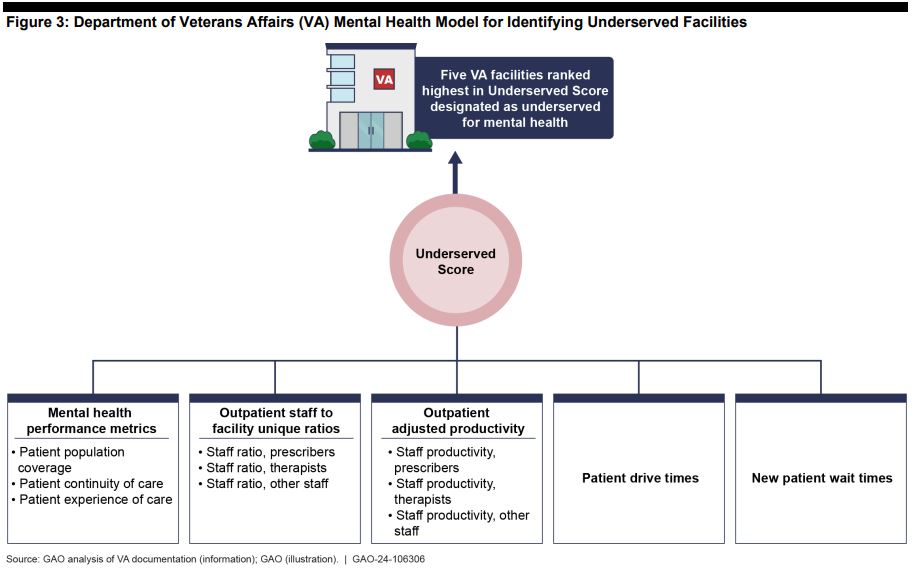
The designation for the Medically Underserved Facility Initiative occurs yearly. For primary care, VA takes into account the number of enrollees served per day, provider availability, community care volume, veteran demographics and enrollee income, average drive time and patient wait time. For mental healthcare, they also look at patient continuity of care, performance metrics and staff ratios and productivity.
Facilities are designated as medically underserved in October, and VISN directors are notified in November. A meeting is held with facility leaders in December, and they are tasked with creating action plans, which are due by the end of January.
Those action plans can include hiring initiatives, increases in telehealth, staff restructuring and other ways to improve patients’ access to care. They also can include structural improvements.
“In 2022, VA reported that its infrastructure required significant modernization to meet modern healthcare standards and provide the services necessary to meet the needs of veterans,” the GAO report notes. “According to VA, some medical facilities may choose a construction project as a strategy to expand space for providing care. Facilities may also take actions such as repurposing or expanding space within existing facilities, moving clinics to different locations, or merging services between facilities located near each other.”
The initiative has received mixed response from the facilities required to take part. One of the most common criticisms is that the action plan items have been things the facility was doing anyway, and the initiative adds another layer of bureaucracy and unnecessary work. Complaints about the time required to oversee the initiative was a running thread through many of the responses. One facility leader described it as an “underfunded mandate” and said “nothing comes of it.”
Another reported shortfall was the lack of support from VA leadership to implement the plans.
“Increased awareness around access challenges prompted focus on developing an action plan to address access, which has been beneficial,” the GAO investigators stated. “However, officials noted that there was no effect on access to care because they have not received additional resources, such as additional support for providing virtual care, to support these actions.”
According to the Office of Integrated Veterans Care (IVC), VA does not allocate resources to facilities based on their underserved status but based on workload. A 2022 VA internal evaluation of the report suggested VA target its resources on those underserved facilities if the department wants to see any substantive change.
“While the various mitigation strategies available are often obvious … actual implementation is far more challenging,” the 2022 report said.
Some VISN and facility leaders agreed about prioritization of funds, stating that they would like to see the underserved designation come with permission to hire more staff and secure additional resources.
Others felt the label should be done away with altogether.
“Some VISN and designated underserved facility officials cited the demoralizing effect of the underserved designation on their facilities,” the report states. “Officials from one VISN pointed to additional challenges with staff recruitment stemming from negative perceptions of the facilities designated as underserved. … [They] suggested removing the undeserved label [and] instead work directly with facilities on underlying access to care issues.”
The 10 facilities given the medically underserved label are not the only ones unable to meet the demands of care for veterans in their system. Other facilities fall within the same range. However, VA has capped the initiative at 10 due to IVC’s limited ability to provide additional resources.

