
VA nurses David Shay, RN, a Marine Corps veteran, left, and Genesis Jalad, RN, are part of the Homeless Patient Aligned Care Team (HPACT) at the West Los Angeles VAMC. A recent report suggested that the VHA is more efficient because it has more registered nurses than the private sector. VA photo
NEW YORK — Several recent studies have shown that VA healthcare is consistently as good as—or better than—non-VA healthcare. Now a study shows VA healthcare is also more efficient.
Study authors Steffie Woolhandler, MD, MPH, and David U. Himmelstein, MD, have long been interested in high administrative costs and waste in the U.S. healthcare system. Having conducted several studies comparing the U.S. administrative costs and personnel to those of other nations, they wondered if there was “any piece of the U.S. healthcare system that looks more administratively efficient than run-of-the-mill places,” Himmelstein said.
Suspecting that the VHA might be different due to its noncommercial nature, the researchers sought out and worked with collaborators in the VA who helped them show their suspicions were correct. Participating in the study were the Office of Productivity, Efficiency, and Staffing, Quality and Patient Safety at the Department of Veterans Affairs in Washington, DC, and the Office of the Chief of Staff at the Boise, ID, VAMC.
In previous studies looking at the occupations of healthcare personnel in the U.S. as compared to other nations, the researchers had developed a classification scheme grouping all of the different occupations in healthcare into categories, of which three are administrative, said Himmelstein, a distinguished professor of public health and health policy in the City University of New York School of Public Health at Hunter College.
The researchers analyzed data on employment and occupation from a Census Bureau survey of 3.2 million Americans and applied the classification criteria to workers in VHA and private-sector hospitals, clinics and medical offices. In addition, collaboration with VA researchers enabled them to include data from the VA central, “which was vital for comparison, because a fair amount of the administrative work of the VA is done in the central office,” Himmelstein said.1
Their cross-sectional study, reported in JAMA Network Open, was conducted using data from 2019, prior to pandemic-related disruptions in healthcare staffing and was carried out between Jan. 14 and Aug. 10, 2023.
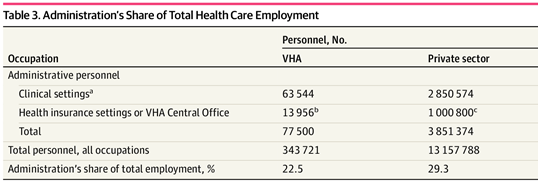
Click to Enlarge: Abbreviation: VHA, Veterans Health Administration.
a. Source: authors’ analysis of the 2019 American Community Survey.
b. Source: authors’ analysis of VHA Personnel Accounting Integrated Data system data.
c. Source: Bureau of Labor Statistics Employment Matrix. Source: JAMA Network Open
Their findings:
- Of the 3,239,553 persons surveyed, 122,315 individuals (weighted population, 12,501,185 individuals) were civilians working in hospitals or ambulatory care; of the weighted population, 12,156,988 individuals (76.2%) were private sector personnel, and 344,197 (63.8%) were federal employees.
- In clinical settings, administrative occupations accounted for 23.4% of private sector vs. 19.8% of VHA personnel.
- After including 1,000,800 employees at private sector health insurers and brokers and 13, 956 VHA Central Office personnel with administrative occupations, administration accounted for 3,851,374 of 13,157,788 private sector employees (29.3%) vs. 77,500 of 343,721 VHA employees (22.5%).
- Physicians represented approximately 7% of personnel in the VHA and private sector, while the VHA deployed more registered nurses (23.7% vs 21.2%) and social service personnel (6.3% vs. 4.9%) than the private sector.
- Fewer Administrative Personnel
The key finding was that, while the VHA employs similar percentages of doctors and nurses compared to the private sector, it employs far fewer administrative personnel as a percentage of its workforce—about a 6 percentage-point difference, Himmelstein said. “This translates to, if the private sector healthcare organizations staffed in the same way as the VA did, they would employ about 900,000 fewer administrative personnel.”
Himmelstein said he and his colleagues went into the study expecting there would be a difference between VA and private sector efficiency, but they didn’t expect the magnitude of the difference they found. “Frankly, because I worked at the VA as a resident many years ago, and I have colleagues who have worked in the VA, our impression is that the VA is pretty bureaucratized,” he said. “So we are a little surprised by how big the differences were.”
Himmelstein noted that the commercial orientation and financing structure of private sector healthcare could be what’s driving the “tremendous administrative inefficiency. Institutions can make more money by hiring more administrators and managers and clerks, but overall it makes the healthcare system much less efficient because those people are doing just money-related tasks that are not necessarily for clinical work. If you could get rid of the crazy financing schemes and drive to run healthcare institutions like a business that maximize their revenues and minimize their expense, we could make our healthcare system more efficient.”
“Not our study, but other studies have found that VA care on average is better than the private sector care,” he added. “There are probably some VA hospitals that are worse and some outstanding private hospitals that are better, but on average, VA care really looks better. So not only is it more efficient, but the patient outcomes look better.”
Last year, a review determined that care provided in the VA healthcare system is consistently as good as or better than non-VA care in terms of clinical quality and safety.
RAND Corp. authors pointed out in the Journal of General Internal Medicine that the studies they reviewed on safety and effectiveness indicated generally favorable performance by VA facilities compared to non-VA facilities, with 22 of 34 studies of safety and 20 of 24 studies of effectiveness showing the same or better quality of care in VA facilities and the remainder showing mixed (four studies) or worse (12 studies) performance.2
This systematic review of compared care provided in VA and non-VA settings and included published studies from 2015 to 2023, updating two prior systematic reviews on this topic.
- Woolhandler, S., Toporek, A., Gao, J., Moran, E., Wilper, A., & Himmelstein, D. U. (2024). Administration’s Share of Personnel in Veterans Health Administration and Private Sector Care. JAMA Network Open, 7(1), e2352104. https://doi.org/10.1001/jamanetworkopen.2023.52104
- O’Hanlon C, Huang C, Sloss E, Anhang et. Al. Price R, Hussey P, Farmer C, Gidengil C. Comparing VA and Non-VA Quality of Care: A Systematic Review. J Gen Intern Med. 2017 Jan;32(1):105-121. doi: 10.1007/s11606-016-3775-2. Epub 2016 Jul 15. PMID: 27422615; PMCID: PMC5215146.
