
Last fall, David Hernandez, MD, (left), a reconstructive surgeon at the Michael E. DeBakey VAMC, performed a microvascular (free flap) reconstructive surgery on a cancer patient. A new review finds care within the nationwide VA Healthcare System is as good or better than community care. VA photo
SANTA MONICA, CA — A new review has determined that care provided in the VA healthcare system is consistently as good as or better than non-VA care in terms of clinical quality and safety.
“Access, cost/efficiency, and patient experience between the two systems are not well studied,” RAND Corp. authors also pointed out. “Further research is needed on these outcomes and on services widely used by Veterans in VA-paid community care, like physical medicine and rehabilitation.”
While consistent with piecemeal studies over the last few years and likely welcome news to the nation’s largest integrated healthcare system, the systematic review published in the Journal of General Internal Medicine also has political implications.1
Due to the VA Choice and MISSION Acts, VA increasingly pays for community care outside of its system in the community. The impetus for Congress to change the laws was not only access issues, but also widespread concerns—whether proven or not—about quality and safety in the care of veterans.
This systematic review compares care provided in VA and non-VA settings and includes published studies from 2015 to 2023, updating two prior systematic reviews on this topic.
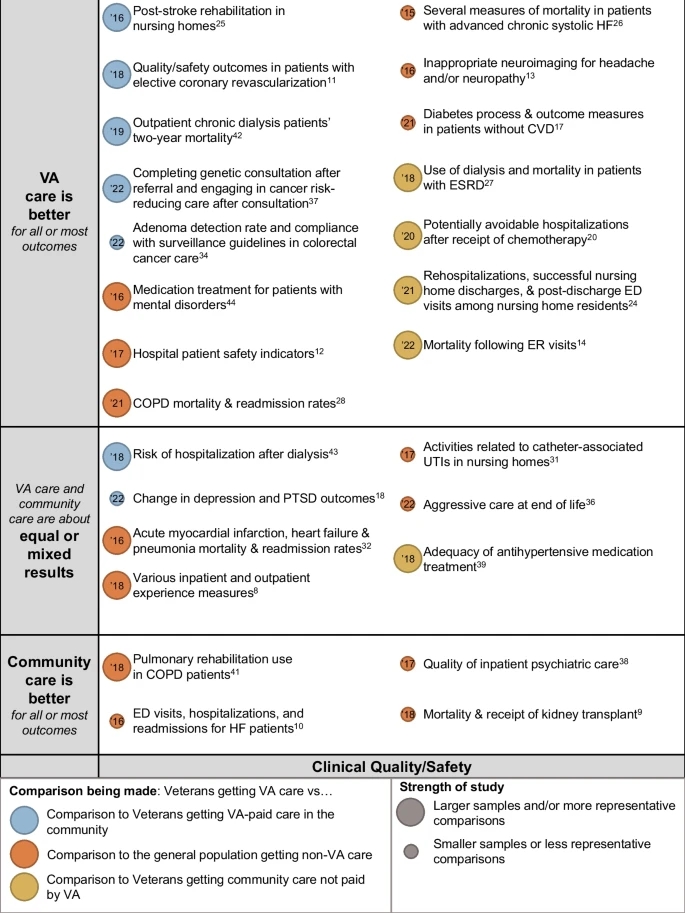
Click to Enlarge: Evidence map of VA vs. non-VA clinical quality/safety. Notes: Studies are listed on the vertical axis by their qualitative results (VA care is better than community care, VA care and community care are about equal, or results are mixed, and community care is better than VA care). Study quality is depicted by bubble size, with larger bubbles being studies of better quality and representativeness than studies depicted by smaller circles. Cont. Source: Journal of General Internal Medicine
The study team searched PubMed, Web of Science and PsychINFO from 2015 to 2023 for published literature comparing VA and non-VA care, including VA-paid community care. Records were included at the abstract or full-text level if they compared VA medical care with that provided in outside healthcare systems. The focus was on clinical quality, safety, access, patient experience, efficiency (cost) or equity outcomes, with data abstracted by two independent reviewers.
After screening 2,415 titles, the researchers included 37 studies—12 comparing VA and VA-paid community care. Most studies assessed clinical quality and safety, although studies of access were the second most common. The study noted that only six studies assessed patient experience, and six assessed cost or efficiency. “Clinical quality and safety of VA care was better than or equal to non-VA care in most studies,” it noted.” Patient experience in VA care was better than or equal to experience in non-VA care in all studies, but access and cost/efficiency outcomes were mixed.
“In keeping with the findings of the prior review, we find that VA is generally more adherent to recommended care processes than other systems of care,” the RAND team wrote. “However, better processes did not necessarily achieve better outcomes, as we observed few differences in adjusted mortality. Although easy to obtain, mortality may not be the optimal outcome for comparison for several reasons, some of which were noted in the prior review. While nearly every study we included attempted to risk-adjust the veteran and non-veteran populations, some excess baseline mortality risk may still be present, since veterans have comparatively worse health status than the general population.”
Since prior reviews with similar results were performed “concerns about access to care led to the Veteran Access, Choice, and Accountability (“Choice”) Act of 2014, which allowed veterans to seek medical care in the community if the VA was unable to schedule a visit within 30 days or if the veteran lived greater than 40 miles from their closest VA,” the article advised. “This program also required independent performance assessments of VA’s healthcare services related to access and available expertise.”
Funding for the Choice Act funding ended in 2017 and was followed by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018 that further addressed concerns regarding veteran access to care by expanding eligibility for VA-reimbursed community care (CC) options.
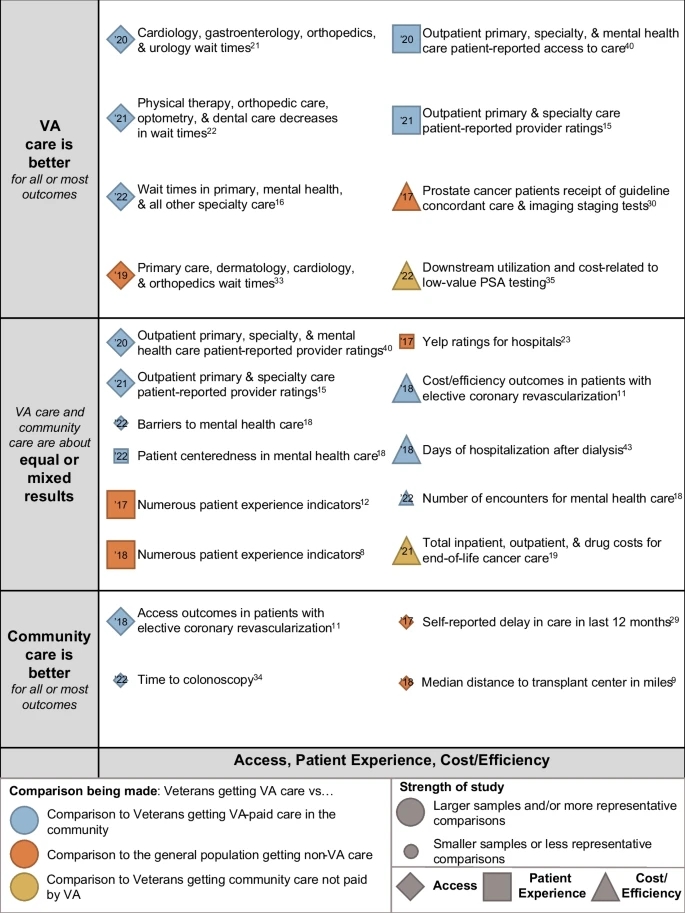
Click to Enlarge: The color of the bubble indicates the type of comparison: blue for studies comparing Veterans getting care from VA to Veterans getting VA-paid care in the community; orange for studies comparing Veterans getting care from VA and non-Veterans, or a general population, getting care in the community; and, yellow for studies comparing Veterans getting care from VA to Veterans getting care in the community not paid for by VA. Beside each circle is a brief annotation of the study topic, and inside the bubble is the year of publication (’18 = 2018,’19 = 2019, etc.). Source: Journal of General Internal Medicine
“These acts greatly expanded the potential for care delivered to veterans and paid for by VA to be from community providers, raising additional questions about comparisons of the quality of healthcare,” the researchers stated. “Unlike prior studies and reviews of prior studies where subjects sorted into VA or non-VA care due to eligibility or preference, there is now the situation where VA is enabling Veterans eligible for VA care to get care outside of VA—community care—at VA’s expense.”
Here are some of the study specifics:
- The researchers said the studies they reviewed on safety and effectiveness indicated generally favorable performance by VA facilities compared to non-VA facilities, with 22 of 34 studies of safety and 20 of 24 studies of effectiveness showing the same or better quality of care in VA facilities and the remainder showing mixed (four studies) or worse (12 studies) performance.
- As for safety alone, the review found that VA facilities performed similarly or better in most, but not all, studies comparing morbidity and mortality. Results from studies about complications and patient safety indicators were more mixed, it noted.
- In terms of effectiveness, VA facilities had similar or superior quality to non-VA facilities when it came to preventive, recommended and end-of-life care, as well as managing medications.
- Nonambulatory care studies indicated similar care quality between VA and non-VA settings. However, studies on service availability had mixed results.
More Studies Needed
While the review had some limitations, the RAND researchers said the available data indicate overall comparable healthcare quality in VA facilities compared with non-VA facilities in terms of safety and effectiveness. “Rates of complications and availability of services had the least favorable results, but these results were mixed rather than consistently poor,” they added, explaining, “The overall number of studies comparing VA and non-VA care was small, and study quality varied. More studies that examine and compare the quality of VA care with respect to timeliness, equity, efficiency, and patient-centeredness are needed to better assess VA facilities’ performance on these quality dimensions.”
- O’Hanlon C, Huang C, Sloss E, Anhang Price R, Hussey P, Farmer C, Gidengil C. Comparing VA and Non-VA Quality of Care: A Systematic Review. J Gen Intern Med. 2017 Jan;32(1):105-121. doi: 10.1007/s11606-016-3775-2. Epub 2016 Jul 15. PMID: 27422615; PMCID: PMC5215146.
