WASHINGTON, DC — Despite suicide prevention being a top priority at VA, clinicians are failing to consistently ask patients at risk for suicide about their access to guns. This inconsistent application of VA’s lethal means safety (LMS) protocols may have resulted in missed opportunities to prevent veterans from taking their own lives, according to a report issued by VA’s Office of the Inspector General (OIG) last month.
In 2019, approximately 69% of veteran suicides involved firearms, compared to 48% in the general population. While firearm-related suicides among non-veterans dropped from 2001 to 2019, they rose 3% among male veterans and 13% among female veterans during that same time period.
Recent studies of firearm-related suicides among veterans and servicemembers have shown that approximately 85% of individuals who attempt suicide with a firearm die from their injury, and the time interval between deciding to act and attempting suicide may be as little as 5 or 10 minutes. These studies have shown that one way to help prevent those suicides is to increase the time between the suicidal thought and the opportunity to act on it. This could be as simple as putting the firearm in a safe or lockbox, or storing firearms unloaded and separate from ammunition.
For years, VA and other healthcare systems have been including lethal means counseling into suicide prevention efforts. In November 2019, the department kicked off a suicide risk identification strategy that included a standardized screening and, if a patient screened positive for suicide risk, comprehensive suicide risk evaluation (CSRE). The CSRE template prompts the clinician to assess the patient’s access to lethal means and, depending on risk level, complete a safety plan.
In addition, VA implemented a nationally standardized safety planning note template that includes documentation of firearms access. VA instructs clinicians to “always ask about access to firearms,” and, if firearm safety was not discussed, document the reason that firearm safety was not discussed. VHA further instructs clinicians to consider “options for improving safe storage,” with patients who report access to firearms.
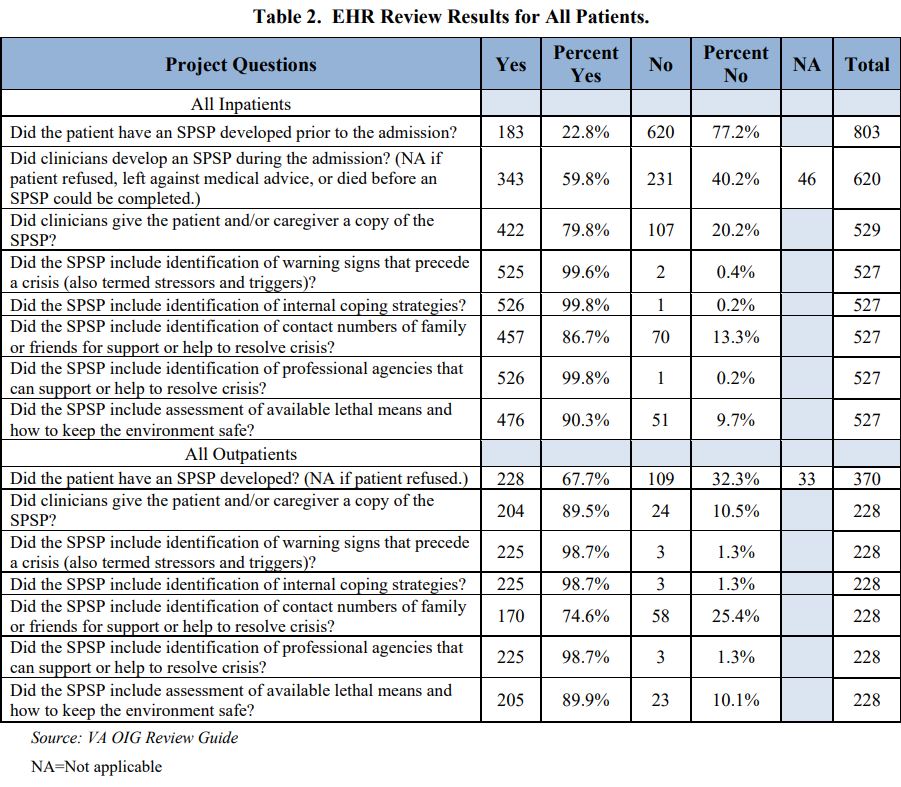
The OIG reviewed the health records of 480 patients who exhibited firearm-related suicidal behavior, 65 of them fatally. Of the 15 patients who required a CSRE prior to the event, three did not have documentation. Of the remaining 12 CSREs, have failed to include firearms access. And of the six suicide risk assessments with documented firearm access, half of those failed to discuss safe storage with the patient.
Safe Storage
“The OIG determined staff failed to include safe storage discussions in approximately 30% of CSRE mitigation plans when patients had reported access to firearms,” the report’s authors state.
During the course of their investigation, the OIG surveyed 3,094 clinicians. Of those, 10% reported not completing the mandatory LMS training, and only one-third reported that the training affected the frequency with which they assessed firearms access and discussed safe storage.
“Most clinicians reported that educational and cultural barriers such as mistrust of authority or government systems, fear of infringement of Second Amendment rights, and reluctance to give up means of self-protection were factors that might impede patient disclosure of firearms access,” OIG investigators explained in their report. “Although LMS training appears to increase clinicians’ confidence that discussions with patients about their firearms access and storage decreases a patient’s suicide risk, educational and cultural factors may continue to be barriers to staff’s engagement in firearms access and safe storage discussions with patients.”
The report goes on to provide a number of recommendations, including that the Under Secretary for Health ensures compliance with training requirements, evaluates the adequacy of the one-time LMS training requirement, and considers initiatives to overcome the cultural barriers in discussions around firearms.
VA Under Secretary for Health Shereef Elnahal, MD, responded to the report, agreeing with OIG’s recommendations.
“Over 70% of veteran suicides are related to firearms. Most suicidal crises are brief, and the time from decision to action can be less than one hour,” he wrote in an addendum to the report. “We can save lives if it takes longer for a person to access the means to harm themselves after the moment they have the impulse to act. Lethal means safety related to firearm secure storage is a critical priority within [VA’s suicide prevention strategy].”
He also noted that, while the LMS-specific training is a one-time-only requirement, LMS is part of VA’s annual course that covers suicide prevention.
“VA has made lethal means safety training a critical focus area,” he said. “[That] includes focus on training of community providers.”