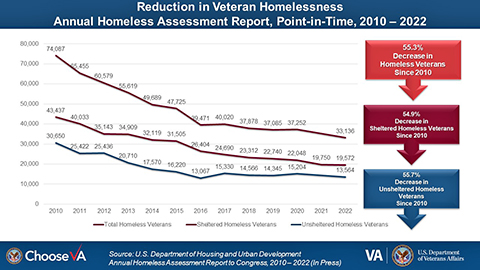
Click to Enlarge: Chart of 55.3% reduction in Veteran homelessness from 2010 to 2022 Source: U.S. Department of Veterans Affairs
SAN ANTONIO — Despite an elevated risk of mental illness and substance use disorder in most homeless populations, a scarcity of research exists on the use of psychiatric medications and understanding of prescribing practices among providers for these populations.
A new study—the latest in a series to examine these issues—found that homeless veterans with mental illness were less likely than housed veterans to be prescribed benzodiazepines yet were more likely to receive “risky and inappropriate” prescriptions for benzodiazepines.
Benzodiazepines are a class of depressant drugs commonly prescribed for conditions including anxiety disorders and insomnia. Although they have held an important role in the treatment of these conditions for more than a half-century, they also have to be carefully prescribed because they can be misused, overdosed, addictive or lead to other adverse events, said Jack Tsai, PhD, MSCP, research director for the VA National Center on Homelessness Among Veterans and professor in the Department of Management, Policy and Community Health at UTHealth School of Public Health San Antonio campus.
“Given the precarious housing situation of homeless populations, it’s important to understand how these important medications are being used, for what disorders they are being prescribed and possible contraindications that need to be considered,” Tsai said.
Tsai’s previous research has included studies on the prescription of antidepressants and antipsychotic medications in homeless veterans. “Through discussions with my colleague, Dr. Katie Koh, a psychiatrist at Harvard, I thought it would be informative for us to conduct a study adding to these classes of medications by focusing on benzodiazepines as well,” he said.
In the new study, using VA administrative data, Tsai and his colleagues used logistic regression to compare the likelihood of benzodiazepine prescribing and t-tests to compare indicators of risk and potentially inappropriate benzodiazepine prescribing patterns for 244,113 homeless service users and more than 2.7 million housed peers.1
“Homeless populations are challenging to study because of their transient nature,” Tsai said. The ability to utilize data within the VA’s comprehensive national healthcare system allowed the researchers to conduct analyses that otherwise would have been impossible. The authors analyzed 2018-2019 data so that the study would be contemporary yet would avoid unique circumstances that may have affected access to psychiatric care during the COVID-19 pandemic in 2020, Tsai said.
Risky and Potentially Inappropriate
Unadjusted analyses showed that benzodiazepines were prescribed for 7.5% of homeless VA service users with mental illness, versus 9.4% of their housed peers. Analyses adjusted for sociodemographic and clinical characteristics and healthcare utilization showed that homeless service users were less likely than their housed peers to receive a benzodiazepine prescription. However, compared with their housed peers, homeless service users received higher rates of risky and potentially inappropriate benzodiazepine prescriptions, including multiple concurrent benzodiazepine prescriptions and concurrent prescriptions for benzodiazepines and opioids or sedatives.
Tsai said he was surprised that the “risky and potentially inappropriate” prescribing of benzodiazepines was higher for homeless veterans, since homeless veterans were less likely to be prescribed benzodiazepines than housed veterans. “While some prescribers are more conservative in prescribing benzodiazepines, since the people experiencing homelessness face many barriers to staying engaged in care, our data suggests there may be some circumstances in which there is less caution in prescribing to homeless veterans than housed veterans,” Tsai advised. “One of the largest differences was the high rate of benzodiazepine prescriptions for homeless veterans over 65, where care needs to be exercised, since there is a high risk for adverse effects. This follows the famous Beers criteria, which recommend that benzodiazepines be avoided in all older adults due to the risk of cognitive impairment, delirium, falls, fractures and car accidents.”
“VA has made significant progress in reducing homelessness among veterans, but it is important that there are proper healthcare services, including medications, that are provided in conjunction with housing assistance to ensure veterans keep their homes and avoid returns to homelessness,” he added.
The new study shows greater education for prescribers on whether and how to prescribe benzodiazepines to homeless populations might be needed, Tsai said. “Integrating prescribers as part of homeless service teams may also be important,” he added. “Hence, they are well-informed of any extenuating circumstances of clients that can inform their prescribing decisions.”
- Koh, KA,Szymkowiak, D, Tsai, J. (2023). Benzodiazepine Prescriptions for Homeless Veterans Affairs Service Users With Mental Illness. Psychiatric services (Washington, DC), appips20220472. Advance online publication. https://doi.org/10.1176/appi.ps.20220472

